INTRODUCTION
Myeloid sarcoma or granulocytic sarcoma is an unusual tumor of immature cells of the myeloid origin8). The tumor is reported in 0.7% to 9.0% of patients with acute or chronic myeloid leukemia (CML) and usually is seen either at the time of initial presentation or during some phase of the disease7). However, in some rare cases, it may present as recurrence of leukemia before it becomes apparent clinically9). Common sites of occurrence are skin, soft tissue, bone, periosteum and lymph nodes, with rare involvement of central nervous system1,12). In spinal involvement, myeloid sarcoma usually occurs as an epidural mass with signs of cord compression6,7,16). However, a few cases of rare intramedullary involvement have been reported worldwidely2,9,15). We report an extremely rare case of intramedullary myeloid sarcoma in a patient with CML as a hematologic relapse.
CASE REPORT
A 58-year-old male was transferred to neurology division under the diagnosis of suspicious acute transverse myelitis. He suffered from progressive paraparesis and voiding difficulty for several months. The patient had a medical history of CML and underwent allogenic bone marrow transplantation 13 years ago. He had complete remission from the disease and had no neurological deterioration.
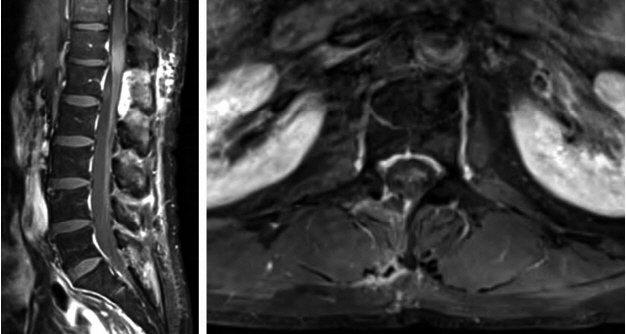
The patient developed sudden both lower extremities weakness and gait disturbance without any trauma history. He was treated with conservative treatment in local clinic for several month but the symptom was aggravated with newly developed urinary and defecation difficulties. He was transferred to tertiary medical center for the further treatment. Initial magnetic resonance imaging (MRI) with gadolinium enhancement revealed an about 3 cm sized intramedullary lesion with slight T2 hyperintensity and mild homogeneous enhancement at T12-L1 level (Fig. 1). Open biopsy with cerebrospinal fluid cytology study was negative for malignancy, hematologic disorders and infection. His final diagnosis was acute transverse myelitis and was treated with high-dose steroid injection and plasmaparesis for 7 days without any neurological improvement. He was then transferred to rehabilitation center for 2 month of comprehensive rehabilitation and physical therapy. His neurological symptom worsened gradually against all efforts and was consulted to our institution for the second opinion.
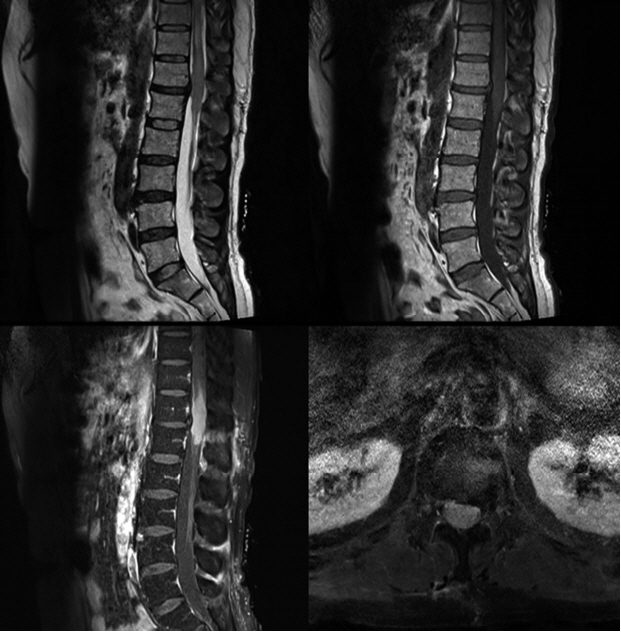
Initial neurological examination demonstrated grade I motor weakness of both lower extremities and severe hypesthesia below L1 dermatome without any long tract signs. Laboratory examination revealed mild lymphocytosis (52.8%) without any sign of hematologic disorder or infection. Enhanced spinal MRI after the admission showed increase in size of intramedullary enhancing mass lesion with newly noted syrinx and postoperative change at T12-L1 level (Fig. 2). Our initial impression was granulocytic sarcoma or atypical infectious myelitis.
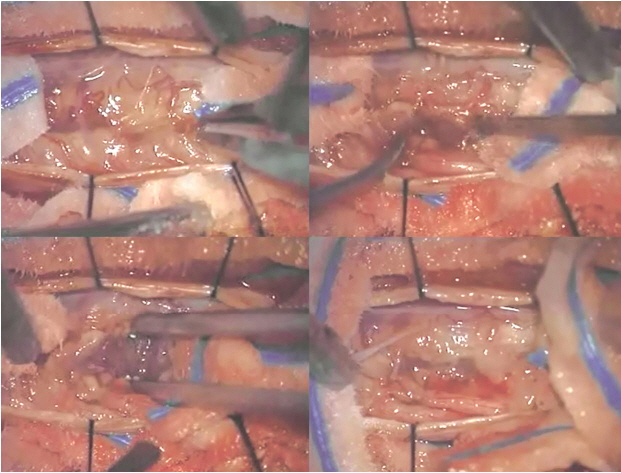
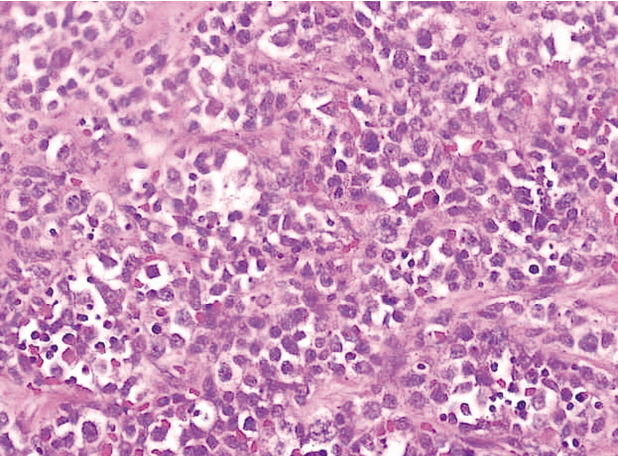
Patient was consulted to the neurosurgery department for the open biopsy. Extended T12 laminectomy and mid-line myelotomy with open biopsy was done under general anesthesia (Fig. 3). Frozen biopsy revealed malignancy with atypical small round cells. There was no complication related to the operations (Fig. 4). Final pathologic confirmation was myeloid sarcoma with 80% Ki-67 and positive CD117 in immunohistochemistry. Histologic findings suggested presence of numerous blasts with round or oval nucleus, dispersed chromatin and prominent nucleolus. The cytoplasm of the majority of neoplastic cells was agranular with a varying degree of basophilia. Eosinophilic granulation was notable in a minority of a cell population (Fig. 5). After histologic confirmation the patient was transferred to hematologic department for the further treatment.
DISCUSSION
Myeloid sarcoma was first described in 1,811 and represents a rare hematologic phenomenon which occurs in patients with myeloid leukemia3,12). The prevalence of myeloid sarcoma in the spine is estimated to be less than 1% among all patients with acute and CML. All levels of the spine can be affected, but more frequently in the lumbosacral spine, followed by the thoracic spine and cervical level7,15-17). The clinical manifestation of spinal myeloid sarcoma varies, and it largely depends on the tumor location and size4,5,9,14). Most spinal myeloid sarcoma that arises in the epidural or paraspinal tissues can present with signs of cord compression due to mass effect2,9,11). In the presented case, the patient’s initial presentation was paraparesis due to unusual intramedullary location. This unspecific presentation could easily be misdiagnosed with atypical inflammatory condition such as acute transverse myelitis and demyelinating diseases, which could lead to prolonged and inappropriate treatment and delay the timely diagnosis5,7,12,16).
The diagnosis of spinal myeloid sarcoma is often challenging because the clinical and laboratory findings are usually not contributory5,10). The radiologic findings are usually non-specific, and the mass often appears as a soft tissue mass2). On MRI examination, spinal myeloid sarcoma yields a similar signal intensity to muscle on T1-weighted images (WIs) and intermediate signal intensity on T2-WIs with subtle to intermediate enhancement with Gadolinium1,4,14). Immunohistochemistry is the most accurate method for establishing the diagnosis of myeloid sarcoma, and a series of markers can be used for diagnosis confirmation and further lineage characterization6,9,15,16).
Myeloid sarcoma can rarely occur in patients without any evidence of leukemia and may precede the development of systemic disease5,9). If the patient has established leukemia, the diagnosis of myeloid sarcoma is relatively easy and it is suggested to always be included in the differential diagnosis for patients with leukemia with a soft tissue mass6,13). The diagnosis of myeloid sarcoma could be difficult if there is no clinical history of leukemia and every effort should be made to obtain a pathologic diagnosis4,7,9). In the present case, the patient underwent repeated open biopsy and immunohistochemical stains showed positive staining in the atypical, which helped to confirm the diagnosis.
The treatment strategy for myeloid sarcoma largely depends on systemic manifestation of leukemic cells and whether it is initial diagnosis or relapse6,15-17). The optimal timing and treatment of isolated myeloid sarcoma is still controversial, however, delayed or inadequate systemic treatment will almost always progress to systemic infiltrations6,8,10,14). For the patient with myeloid sarcoma who presents with concurrent marrow involvement, systemic treatment is always suggested5,9,16). Overall, prompt diagnosis and adequate systemic treatment are essential for a good outcome.
CONCLUSION
We report a rare case of spinal intramedullary myeloid sarcoma presenting as relapse of CML. Diagnosis may be difficult and knowledge of its clinical presentation, imaging, and histologic characterization can lead to proper diagnosis and appropriate treatment. Although rare, myeloid sarcoma should be prominent in the differential diagnosis whenever a history of leukemia is present in a patient presenting with myelopathy symptoms and unusual intramedullary mass-like lesion.