INTRODUCTION
Ventriculoperitoneal shunt (VPS) is commonly used to treat hydrocephalus. There are a number of complications associated with VPS, such as shunt obstruction, shunt fracture, disconnection, migration, misplacement, over-drainage, and abdominal complications3). One of the complications, abdominal pseudocyst, refers to localized fluid collection around the distal catheter surrounded by non-epithelium cell9). The purpose of this case is to report a delayed abdominal pseudocyst in patients with cysticercosis after VPS.
CASE REPORT
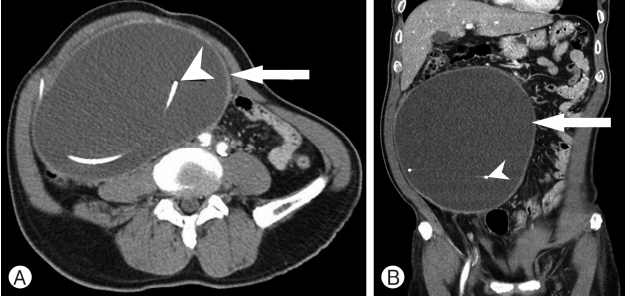
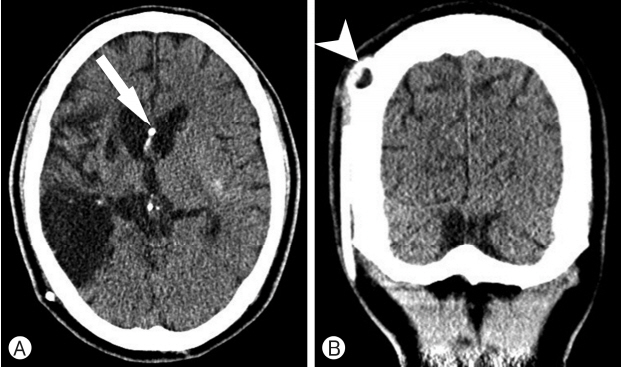
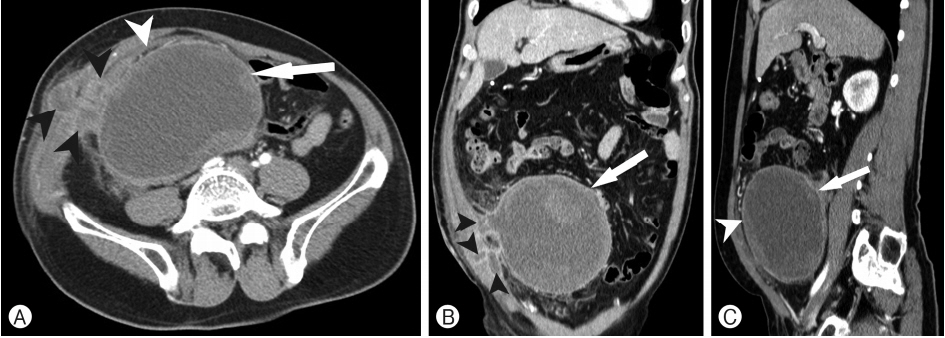
Our patient was a 59-year-old man, who had a VPS operation (PS Medical® medium pressure valve; Medtronic, Minneapolis, MN, USA) for the treatment of hydrocephalus due to cysticercosis 26 years prior to visiting our hospital. About seven years prior, he reported having felt increasing abdominal distention, however he did not visit any hospital. About 1 week prior, he was admitted to the emergency department of another hospital with increased abdominal distention. Abdominal computed tomography (CT) scan and brain CT scan were performed in the other hospital’s emergency department, then the patient was transferred to our hospital. Abdominal CT scan showed well enhanced demarcated fluid collection about 20×18 cm around the distal catheter tip with no evidence of abdominal comorbidities (Fig. 1). The hydrocephalus was observed on initial brain CT scan (Evans index, 0.31) (Fig. 2). In addition, the patient did not exhibit any neurological symptoms (Glasgow Coma Scale, E4V5M6) and laboratory examinations showed no any abnormalities beyond elevated serum C-reactive protein (CRP; 3.10 mg/dL). Serum immunoglobulin E level was normal as well (88.6 kU/L). Also, the result of specific serum immunoglobulin G (IgG) antibody of cysticercosis was negative.
We performed the exploratory laparoscopy and drainage catheter insertion into the abdominal cyst with a general surgery team after reposition of the distal shunt catheter. The cerebrospinal fluid (CSF) analysis from distal tip and abdominal cystic fluid analysis from pseudocyst were performed. The pseudocyst fluid was of a chocolate color. Cytology studies, however, were negative for malignant cells. Additionally, the CSF fluid and abdominal cystic fluid culturing were performed. However, the results of culturing were negative. An India ink test and crypto antigen test was also negative. Polymerase chain reaction for Mycobacterium tuberculosis was negative as well. After the placement of a drain to abdominal cyst, the drain continued to produce up to about 30 to 40 cc of serosanguineous fluid each day. Anthelmintics were not used because specific IgG antibody of cysticercosis in serum and abdominal cystic fluid were negative level. Over the course of the next eight weeks, abdominal CT demonstrated that the pseudocyst decreased (Fig. 3).
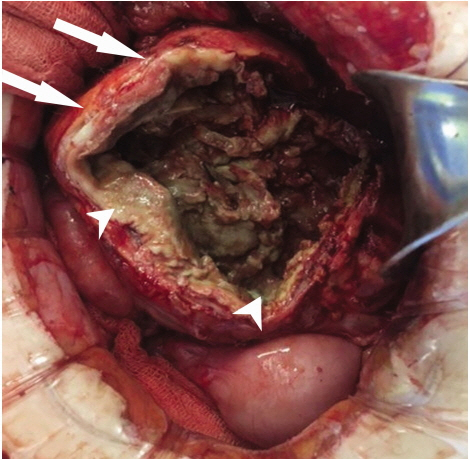
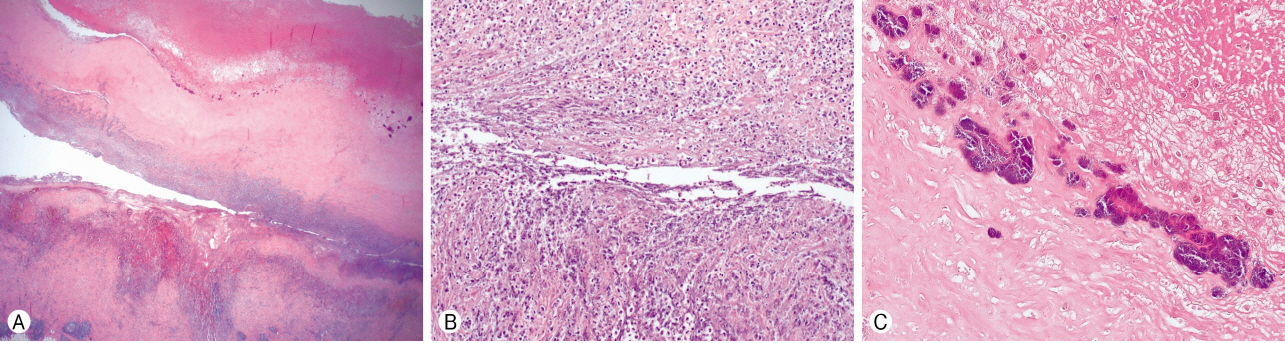
Following drainage catheter removal, pseudocyst was increased again on abdominal CT. A catheter drainage re-insertion and Taurolin® (Taurolidine; Samjin Pharmaceutical Co., Seoul, Korea) solution irrigation (100 cc at once every week) were performed for 3 months, after which pseudocyst size was improved. Three months later, the patient complained of fever, abdominal pain and distension with abdominal tenderness. Follow up abdominal CT showed both that pseudocyst was increased and doubted cystic infection (Fig. 4). The drainage fluid has foul odor and infection was suspected in blood test included white blood cell count (12,380/mm3), CRP (17.54 mg/dL), and erythrocyte sedimentation rate (70 mm/h). An exploratory laparotomy and cyst resection were performed by a general surgery team. Cystic mass was filled with pus-like fluid and had extreme tissue adhesion with peritoneum, omentum, cecum, and small bowel (Fig. 5). Pathology of biopsy revealed the fibrocollagenous tissue with chronic active inflammation, necrosis, abscess formation, and dystrophic calcification on focal findings (Fig. 6). The Methicillin-sensitive Staphylococcus aureus (MSSA) strain was cultured from pus-like fluid. Triaxone® (Ceftriaxone; Hanmi Pharmaceutical Co., Ltd., Seoul, Korea) 2g intravenous injection (IV) and Trizele® (Metronidazole; JW Pharmaceutical., Seoul, Korea) 1.5g IV were used as initial antibiotics after surgery and Cefazoline® (Cefazolin; Chong Kun Dang Pharmaceutical Co., Seoul, Korea) 6g IV was used for 7 days after MSSA was cultured. After discharge, Amoxclan Duo® (Amoxicillin and Clavulanic Acid; Hanmi Pharmaceutical Co.) 2g per oral was used for 3 weeks. Thereafter, we have continued to observe him for 13 months, and he has been without further symptoms to this point.
DISCUSSION
VPS is a commonly accepted surgical technique for the treatment of hydrocephalus. VPS has several associated complications, with rates as high as 40% by 1 year and 50% by 2 years4). The most common complications of VPS are obstruction, infection, and mechanical failure3). Early shunt malfunctions are usually caused by misplacement, disconnection, or migration of the shunt components. The delayed complications of VPS are shunt fracture, over-drainage, loculation of the ventricles, and abdominal complications3).
Abdominal associated complications are ascites, pseudocyst, perforations, etc., while common symptoms of shunt malfunction are nausea, vomiting, irritability, fever, or an altered level of consciousness4). Neurologic examination can identify papilledema, cranial nerve palsies, hyperactive reflexes, and ataxic gait. Abdominal palpation is useful in confirming ascites or an intra-abdominal mass-like lesion. In this case report, the patient presented with increased abdominal distention and abdominal cyst was discovered on the abdominal CT scan. Pseudocysts, which are cases of loculated intra-abdominal fluid collection around the peritoneal catheter, were first reported by Harsh5) in 1954. Abdominal pseudocyst formation occurs in 0.33% to 6.8% of shunt procedures due to abdominal infection6,8). Pseudocysts are more common than ascites, and they present as a localized abdominal mass. Thus, patients with pseudocysts sometimes complain of abdominal discomfort and diffuse abdominal tenderness. If the pseudocyst is large, symptoms such as bowel obstruction may appear2).
The exact pathogenesis of abdominal pseudocyst remains unknown6). Nevertheless, three causes are considered: (1) Chronic infection; (2) Particle like protein in CSF; and (3) Foreign body reaction. Tomiyama et al.10) proposed that the development of pseudocyst suggests the presence of a chronic low-grade infection. However, it is not uncommon to find sterile fluid within the pseudocyst cavity when it is aspirated. Likewise, there is no evidence of any infection in this case report. In the case of children, patients with brain tumors who have VPS placed are more likely to develop pseudocysts, perhaps because of the elevated protein in the CSF interfering with abdominal absorption1,2). According to Pinto and de Oliveira7), VPS catheter is a foreign body that can cause infection or other foreign body reactions, resulting in epithelial responses which may lead to inflammation and obstruction. Other causes (such as a history of abdominal operations, abnormalities of the ascites, and silicon allergies) have also been reported.
Our adult case exhibited onset 26 years after VPS surgery. This case is considered to be an extremely a rare case of abdominal pseudocyst, because abdominal pseudocyst typically occurs 3 weeks to 5 years after VPS surgery in younger patients1). Thus, it is important to consider an abdominal pseudocyst in adults as a candidate cause of acute malfunction of a VPS system, even when more than 5 years have passed since the operation. Also, more aggressive treatment such as direct cyst removal was needed, because keeping the drainage catheter for a long time was cause of the infection.
CONCLUSION
Although the occurrence of pseudocyst after VPS surgery is a rare complication, it can cause additional complications such as obstruction and infection. If patient has gastrointestinal symptoms, pseudocyst should be considered as one of the possible complications of VPS surgery. Even in the case that the patient reports no major problems for a long time after surgery, complications may still occur, even after over 20 years as in our case report, so periodic examination and observation are needed.