INTRODUCTION
Metastatic spinal tumors can cause back pain and paralysis by invading the spinal canal, which can result in pathologic fractures. Such fractures require spondylectomy with reconstruction using mesh cages1). However, thus far, no reports have described the use of customized instrumentation for treating metastatic spinal tumors.
Traumatic compression fractures can cause back pain and limb numbness, specifically when the spinal canal is involved. When a compression fracture progresses, spinal stenosis and kyphosis can occur, and surgery for deformity correction is often required. In such cases, a mesh cage can support the reconstruction of the compressed vertebra after vertebral column resection (VCR) has been completed.
This study reports two cases wherein 3-dimensional (3D) mesh cages were constructed and used to treat a 75-year-old man with a metastatic pathologic fracture and severe paralysis and a 63-year-old woman with severe kyphosis and T11-L1 compression fracture. Herein, we document the approach to the treatment of these two cases using 3D-printed mesh cage. This is the first case of a patient with a metastatic spinal tumor receiving such treatment in Korea. The accumulation of similar case reports is required to increase the uptake of 3D-printed mesh cages in this context.
CASE REPORT
Case 1
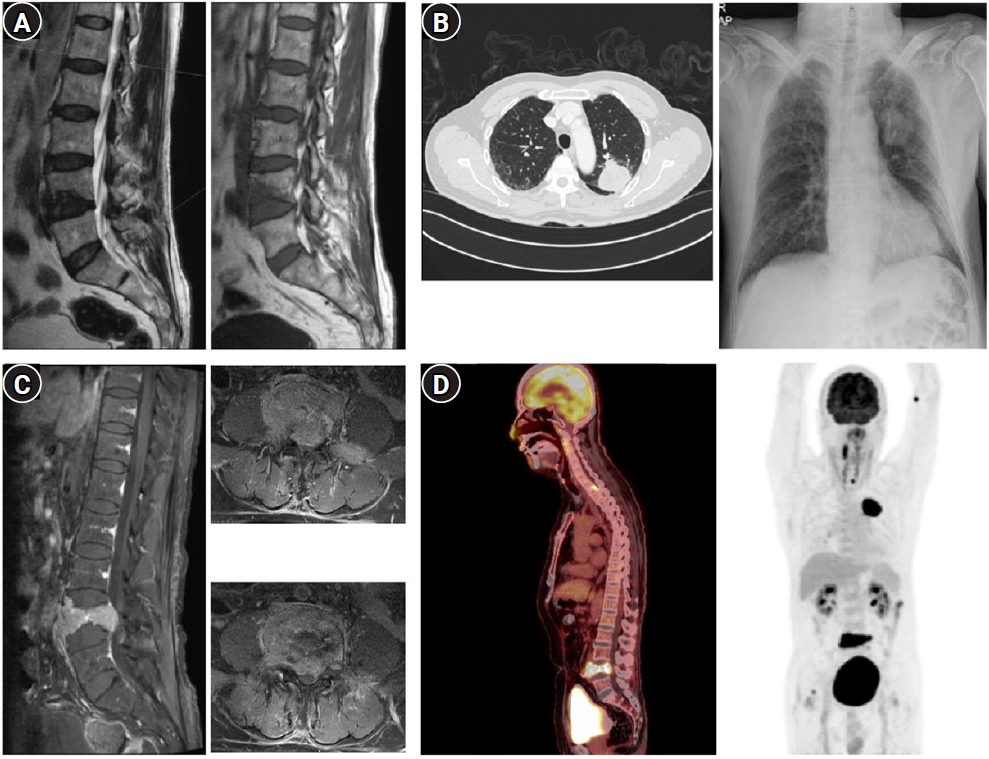
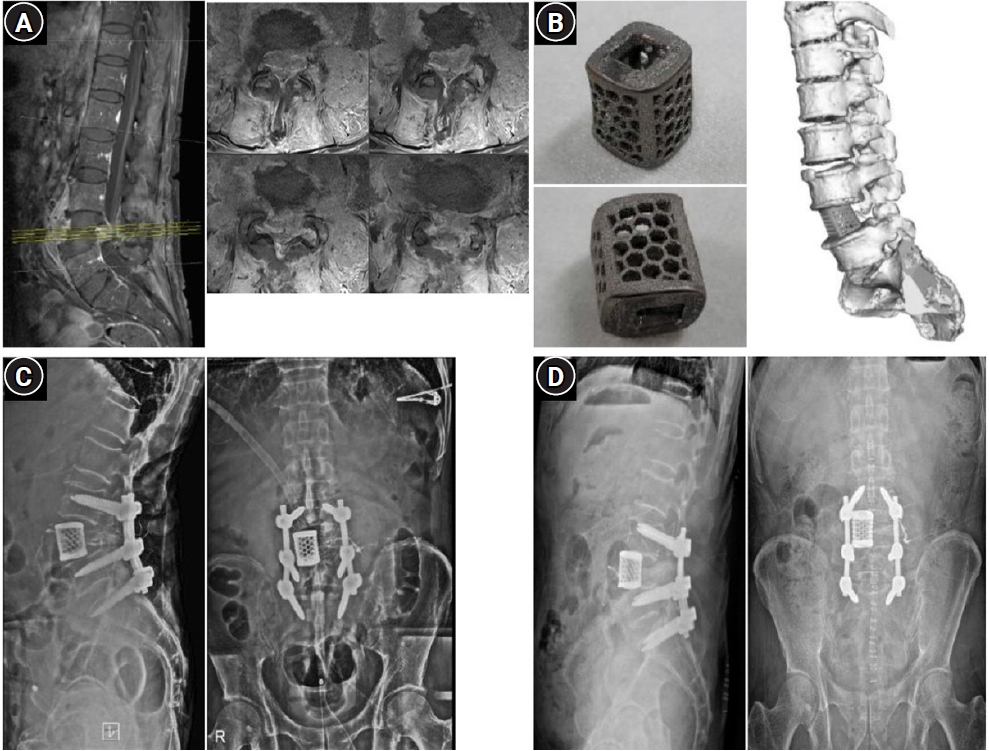
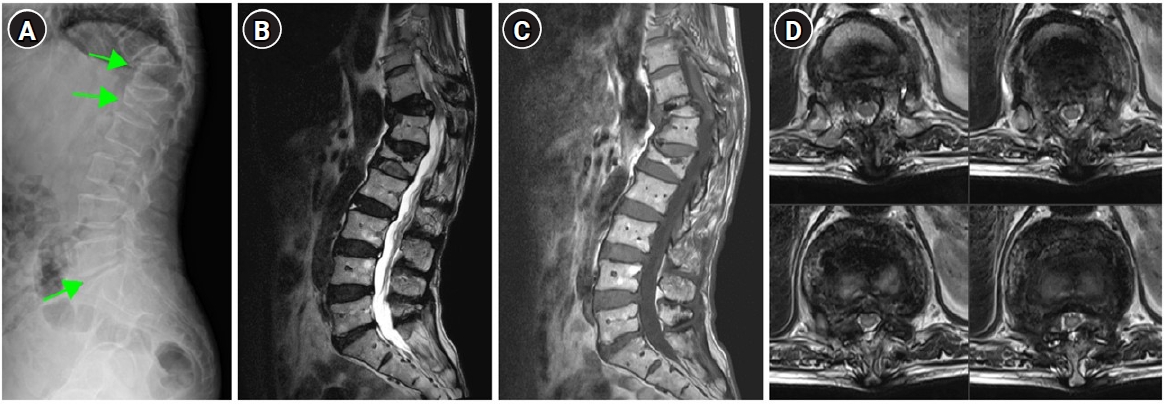
The patient was a 75-year-old man without any relevant medical history. He presented with low back pain and bilateral buttock pain (numeric rating scale [NRS] score of 4 points; wherein 0 to 10 points denoted no pain to extreme pain, respectively), which had persisted since July 2021. Magnetic resonance imaging (MRI) at another hospital revealed an L4-compression fracture (Fig. 1A) followed by sudden weakness and pain in his right leg and L3-L4 dermatome (NRS 7 points) after 6 weeks; subsequently, he presented at our emergency department. The patient had a walking disability and grade IV motor weakness in his right hip, which was otherwise intact. He was admitted to our hospital after plain radiography and contrast-enhanced computed tomography (CT) scans showed a mass-like lesion in the left upper lobe (LUL) (Fig. 1B). The following tumor markers showed elevated levels: carcinoembryonic antigen, 112 ng/mL; carbohydrate antigen 19-9, 53.9 U/mL; and cytokeratin fragment 21-1, 10.6 ng/mL. Contrast-enhanced MRI scanning performed the day after admission showed extraosseous extension, spinal canal stenosis, and a pathologic compression fracture (Fig. 1C) by enhancement at the L4 level. CT-guided bone biopsy at the L4 level revealed a metastatic lesion of non-small cell lung carcinoma (NSCLC). Positron emission tomography-CT scan showed uptake in the LUL, L4 body, and T1 body (Fig. 1D). CT-guided needle aspiration biopsy of the LUL and subsequent histopathologic evaluation confirmed the lesion as a grade IV, B-type Raf kinase-negative, and epidermal growth factor receptor-negative NSCLC. Considering the patient’s lung cancer stage and poor general condition (Eastern Cooperative Oncology Group grade 3), palliative, L4-limited decompression was performed using the posterior approach under general anesthesia. His leg pain reduced (NRS 3 points), and he resumed walker-assisted ambulation. His cancer treatment was continued with once-daily radiotherapy (600 Gy each time) sessions. On the day after the first radiation therapy session, worsening leg pain (NRS 6 points) occurred, which was visualized as an exacerbation of L4 metastasis with severe stenosis (Fig. 2A) on MRI scans. Chemotherapy with Alimta (810 mg) and cisplatin (121.5 mg) was initiated while contemplating the need for additional surgery.
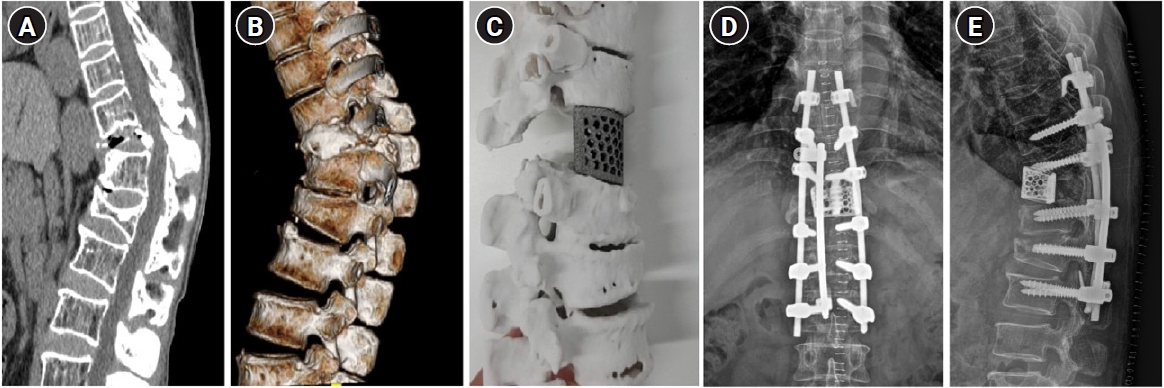
Six days later, which was 2 days after the embolization of L3-L4 spinal arteries, L4-spondylectomy and L3-S1 posterior screw fixation were performed using a customized 3D-printed mesh cage (Fig. 2B) for efficient weight-bearing and lordotic-curve preservation. The leg pain improved (NRS 3 points), and the patient resumed walker ambulation. The second chemotherapy treatment was performed 2 weeks later, followed by additional radiotherapy performed daily on the T1-T2 spine (500 Gy each time). The patient underwent the third chemotherapy session three weeks later (December 15), and his leg pain improved further (NRS 2 points). He remains under general hospital care (February 2022) to drain wound fluid, manage leukopenia, and undergo further chemotherapy.
Case 2
The patient was a 63-year-old woman without any documented medical history. Approximately 13 years ago, she slipped and experienced aggravating back pain 3 months later. Subsequently, T11-L1 compression fracture was diagnosed and managed with conservative care, and her pain subsided. Her back pain resurfaced 6 months before presentation, when she lifted a heavy object and had numbness in both soles of the feet and a cold sensation in the legs, resulting in gait disturbance. She visited the emergency room and received conservative care through the outpatient clinic. No motor deficit was observed, but hypoesthesia was present in both feet. No abnormal deep tendon reflex was observed. Plain radiography (Fig. 3A), CT (Fig. 4A, B), and MRI (Fig. 3B-D) findings revealed severe compression fracture at the T11-L1 level that caused severe kyphosis and stenosis in the thoracolumbar junction. Her symptoms worsened and she was admitted for surgical repair of the spinal deformity. After screw insertion from T9 to L2, total laminectomy of T11 was performed with VCR (grade V osteotomy) following the pedicles. In the empty space after VCR, a 3D-printed titanium mesh cage (Fig. 4C) was inserted. Rods were connected using a domino and a T8 hook, and the surgery was completed without changes in the motor evoked potentials. There was severe postoperative pain, which required pain control medications followed by a slow walking ability. Postoperative plain radiography (Fig. 4D, E) showed a stable cage position. She was discharged on postoperative day 15. During follow-up visits at 1, 4, and 7 months, she showed stability while walking without evidence of dislocations or mechanical failure on her X-rays. Written informed consent was obtained from the patients for the publication of the case report and accompanying images. The study adhered to the Declaration of Helsinki and was approved by the appropriate Institutional Review Board (redacted for peer review).
DISCUSSION
Metastatic spinal tumors can cause pain and lower-limb weakness. Surgery, radiotherapy, or chemotherapy is required independently or in combination to treat such tumors. Spondylectomy with cage insertion and posterior screw fixation using a Harms cage is common1). However, the cylindrical structure of the cage causes problems in its fitting between the non-parallel endplates, resulting in misalignments or dislocation4).
A previous report presented successful outcomes of the application of 3D-printed custom implants for severe bone loss, limb and joint arthrodesis, and spine surgery3). Our case experiences showed that a 3D-printed mesh cage was useful as a replacement after spondylectomy for a metastatic spinal tumor and after VCR for a severe compression fracture. To the best of our knowledge, our experience of such a treatment approach for a patient with metastatic spinal tumor is the first in Korea, wherein a customized titanium 3D-printed mesh cage was used. A 3D rendering model was made based on the patients’ CT scans. After removing the defect region, two 3D planes were formed between the endplates. The rendering model was reduced, as required (in case 2). The modeling of the 3D implant was performed between two planes. Pyramid-shaped spikes were added to the surface meeting the endplate to increase the fixation force.
The angle of the cage surface could be customized in the intervertebral space, given the angle between endplates required for efficient weight-bearing, a strength of a 3D-printed cage. The use of 3D-printed implants can be expanded for indications in spinal oncology, helping achieve tailored/precise treatment.
Furthermore, we concluded that a 3D-printed mesh cage is useful as a vertebral body replacement in severe compression fractures that can cause kyphosis. In our patient, the vertebral body had nearly collapsed due to severe compression fracture, losing its original structure. After the VCR of T11, the mesh cage was needed to compensate for the residual gap and correct the kyphosis. The 3D-printed mesh cage was constructed after considering the height between adjacent vertebral bodies and the angle between two adjacent endplates, and to ensure a tight fit for kyphosis correction. Given the good fit and no observed displacement, the 3D-printed mesh cage may be a good option for deformity surgeries.
The 3D-printed mesh cage device had certain limitations. Although the cage was customized, there were residual fitting issues, and the cage was slightly dislocated in the forward direction over time (Fig. 2C, D), indicating the need for reimplantation and firm fixation. Expandable cages are advantageous in contexts with fitting challenges5); 3D-printed expandable implants may offer a next-generation solution. However, the production of such cages is less cost-effective and requires more time than the use of readymade cages2). Developments in 3D-printing technology are likely to resolve these limitations in the future.
Reconstruction of metastatic spinal tumors and severe compression fracture using a customized 3D-printed cage showed acceptable results, although fitting problems, manufacturing time, and high costs remain to be managed.