INTRODUCTION
Herpes zoster (HZ) commonly presents with vesicular eruption due to the reactivation of varicella-zoster virus (VZV), especially in elderly patients1-5,9). Approximately 50% of HZ in the United States occurs in people 50 or older. VZV can become latent in the dorsal sensory ganglia without causing any symptoms. Several years after a VZV infection, however, the virus may cause viral infection of the skin when the immune system is compromised1,5).
Segmental zoster paresis (SZP) of the limbs, characterized by focal and asymmetric weakness of the extremity, is reported as a rare complication (0.5%-5% of patients with HZ) of HZ that can lead to the misdiagnosis of other radiculopathy or musculoskeletal problems3). SZP typically occurs two to three weeks after the herpetic skin rash and affects the myotome corresponding to the rash distribution regions1,3). Therefore, any motor involvement by SZP may be difficult to diagnose during the first clinical examination.
Here, we introduce a rare case with severe pain and weakness caused by SZP mimicking cervical disc herniation.
CASE REPORT
A 58-year-old male was admitted to our hospital with constant, sharp, right-sided neck pain and tingling sensation with radiation to the right lateral arm, forearm, thumb, and index finger that had first occurred seven days earlier. The pain intensity was 7 out of 10 on the visual analog scale. On physical examination, he showed decreased hand grasping power (manual motor testing [MMT] 3/5). The power was MMT 5/5 in all other muscle groups of the right upper limb, even the shoulder muscles, and in all muscle groups of the left upper limb. No skin lesions were observed at the first visit to our hospital.
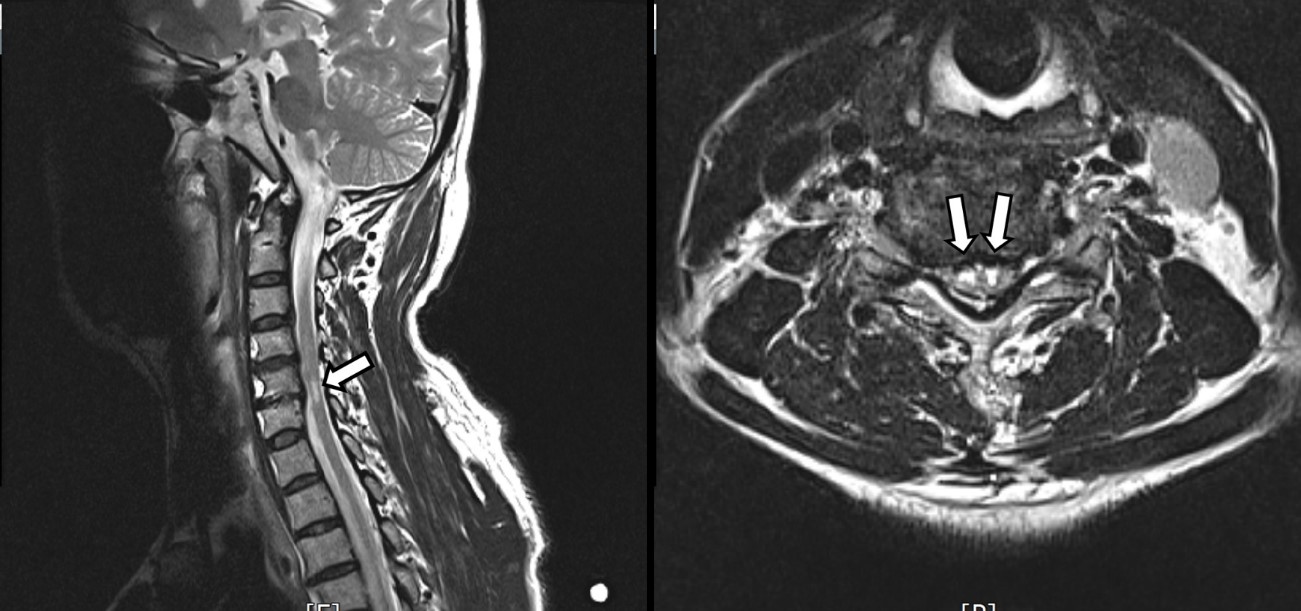
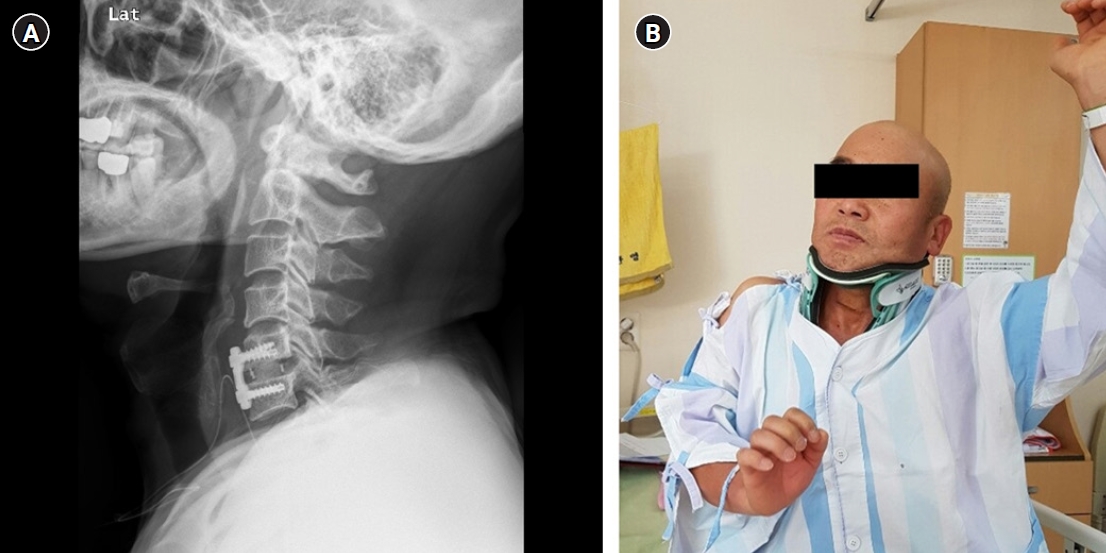
A plain X-ray showed degenerative change with decreased disc height at the C5-6 level (Fig. 1). Magnetic resonance imaging (MRI) showed foraminal stenosis with disc protrusion between the 5th and 6th cervical spine (C5/6) level and a high signal change at the same level of the spinal cord (Fig. 2). There were no abnormalities in his vital signs or lab tests. Thus, we diagnosed the patient with radiculopathy induced by cervical disc herniation with cord injury.
We first treated the patient with oral non-steroidal anti-inflammatory drugs and a computed tomography-guided cervical nerve root block using a mixture of lidocaine and steroid. The next day, however, the patient came back to our emergency room with exacerbated pain. Therefore, we considered anterior cervical discectomy and fusion (ACDF) for the C5/6 level. Still, no skin lesions were found on the patient.
Surgery was performed using the typical ACDF method. The postoperative X-ray confirmed that the disc height increased and was well-fixed by the cage and plate. After surgery, the patient reported a 50% improvement in preoperative pain.
On the second postoperative day, the patient complained of a sudden shoulder drop (Fig. 3A, B). An MRI scan was performed, showing a well-removed disc and decompressed spinal cord and foramen, with no other abnormal findings (Fig. 4).
Motor weakness became worse on the fourth postoperative day, and skin rashes began to appear. On the seventh day, the patient showed complete shoulder drop (MMT grade 1), elbow extension weakness (MMT grade 3), and skin lesions spread throughout the right arm (Fig. 5).
A dermatology consultation was carried out. The patient was diagnosed with HZ in the right C6 dermatome based on clinical findings, including the features of pain (along the C6 area), vesicular rash, and erythema. Antiviral medication was administered and the patient’s symptoms gradually improved.
The patient was discharged from the hospital a month after the surgery, at which time, motor weakness had not fully recovered (MMT grade 3).
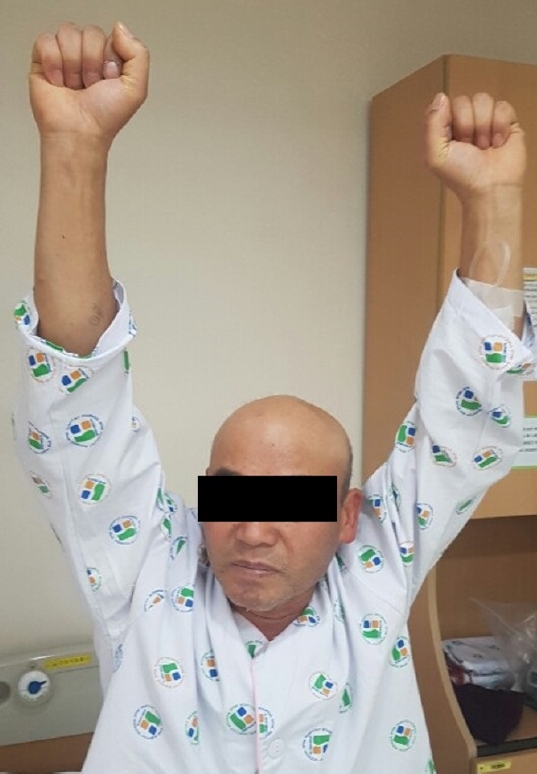
On follow-up, the patient still showed persistent neuropathic pain and weakness. Antiviral drugs were given to the patient after his discharge from the hospital. The patient was also treated with a nerve block to control his pain and rehabilitative therapies for his motor symptoms. Eventually, he was fully recovered six months after surgery (Fig. 6).
DISCUSSION
Varicella-zoster has a high prevalence in people over age 40s, with the highest incidence from ages 60 to 707,8,10). Previous studies reported that the VZV rarely causes SZP, which can involve either nerve roots, the brachial or lumbar plexus, and peripheral nerve lesions. The electrophysiologic and radiologic findings can help to reveal the extent and severity of the affected nerves or nerve roots.
A review of the published papers found that the prevailing opinion is that the disease is more likely to occur in the upper extremities, between the upper and lower limbs, but there is some controversy. Upper limb weakness most frequently occurs at the C5-7 levels, and in the lower extremities, it occurs most commonly at the L1-4 levels. The involvement of the C8 myotome is relatively rare.
The cardinal signs of HZ are skin rash, neuralgia, and rarely, motor symptoms4). Skin lesions generally precede the neurologic symptoms by several days to one week. Some studies reported that in some rare incidents, neurologic symptoms occurred before skin lesions1-3,6-8). The patient in our case also experienced neuralgia followed by skin lesions occurring one week later. This led to our misdiagnosis6).
Imaging abnormalities such as nerve swelling and T2 high signal intensity can be found not only in HZ but also in peripheral neuropathy caused by other diseases such as neurobrucellosis. However, such imaging abnormalities are not found in all patients. Previous studies reported that such abnormalities were found in about 70% of patients10). In our case, the MRI scan revealed a high signal change in the spinal cord. However, it led us to misdiagnose the patient with acute cervical disc rupture accompanied by cord injury rather than SZP.
Several reports have described the differential diagnosis between HZ infection and spinal radiculopathy. Some authors reported that spinal radiculopathy could be ruled out if there are no abnormal MRI findings in the spine10). Therefore, if skin rash symptoms are not evident, careful history-taking of both the nature of the pain and changes in the sensory and motor symptoms are needed to distinguish herpes infection from spinal radiculopathy.
Other papers reported that peripheral neuropathy caused by HZ with predominant axonopathy could be seen in an electrophysiological study5). These include low amplitudes of compound motor action potential or sensory nerve action potential (SNAP), normal or mildly slow nerve conduction study and distal motor latency, and above 35 m/s of nerve conduction velocity. VZV affects the dorsal root ganglion after the initial HZ eruption. Therefore, it is logical that the SNAP amplitudes are low, showing signals of sensory neuron or axon damage. According to existing pathologic studies, demyelination, axon degeneration, and lymphocyte infiltration can be found in the affected nerves, dorsal root ganglions, and dorsal horns. These electrophysiological results appear more than two weeks after weakness begins to occur. Nonetheless, in this case report, we regret that we did not perform electromyography before surgery, even though its use is still controversial.
SZP is an unusual complication of VZV, which shows skin rashes prior to motor weakness. In a few cases, including ours, motor weakness appeared before skin lesions, leading to a misdiagnosis. In the elderly, immunocompromised, or ex-herpetic patients with focal weakness of the extremity and severe pain, one should consider the possibility of SZP even if there are no typical skin lesions of HZ.