Lee, Bock, Sheen, Han, and Sohn: Thoracic Spinal Angiolipoma: A Case Report and Literature Review
Abstract
Spinal angiolipoma (SAL) is a rare benign tumor, accounting for 0.14% to 1.2% of all spinal tumors and approximately 3% of epidural spinal tumors. SAL is composed of mature adipocytes and abnormal blood vessels. Its gradual growth can cause spinal cord and root compression. No additional treatment is required after total surgical resection, and its prognosis is good. We report the c case of an 81-year-old man who had thigh pain and numbness in both feet, along with gait disturbance. High signal intensity was observed on T2- and T1-weighted magnetic resonance imaging. Contrast enhancement showed a highly contrasting epidural mass with spinal cord compression, spreading to the left neural foramen. The tumor was totally removed by laminectomy and facetectomy. After surgery, the patient’s symptoms gradually improved, and a pathological examination concluded that the tumor was an angiolipoma. SAL is an uncommon benign tumor, for which total surgical excision is the treatment of choice.
Key words:
Angiolipoma; Epidural neoplasms; Epidural space; Spinal neoplasms
Angiolipoma; Epidural neoplasms; Epidural space; Spinal neoplasms
INTRODUCTION
Spinal angiolipoma (SAL) occurs in approximately 0.04% to 1.2% of all spinal tumors 17,23,28,30,32,37). SAL is a benign tumor made up of adipose tissues and vasculature 1,16,22,23,27-30,32,34,35,38,39,42). Although the tumor is usually found within the thoracic epidural space, SAL is sometimes found within the lumbar epidural space. It is also found within the cervical and sacral epidural space, though rarely 9,18,32,35,38). Usually, SAL grows slowly and compresses the spinal cord or root, causing symptoms gradually 4,12,18,31,40,46). SAL can be subdivided into two types, non-infiltrating and infiltrating 1,18,23,32,33,35,40). The non-infiltrating type of SAL is easily dissected from the surrounding dura and adjacent tissue because it is encapsulated. In contrast, the infiltrating type is not encapsulated, making total removal difficult 1,23,33,39,42). Magnetic resonance imaging (MRI) has an important role in diagnosing SAL, but the gold standard for diagnosis is pathological diagnosis 1,4,18,23,32,38). The main treatment in SAL cases is surgical removal. Even when infiltrating type is subtotally removed, the prognosis is good 18,27,33,39,40). We report a case of a patient with SAL complaining of cord compression symptoms arising from the thoracic level.
CASE REPORT
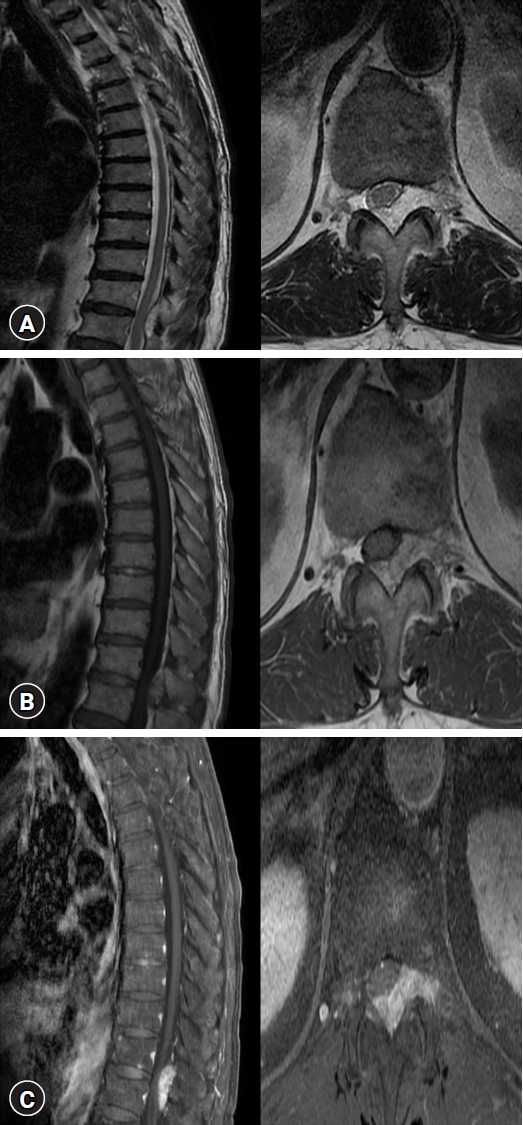
An 81-year-old male patient came to our clinic complaining of numbness in both legs lasting one year. The patient complained of both thigh pain and numbness in both feet. His big toe dorsiflexion motor grades (both toes) were 3+ with gait disturbance. The diagnosis was difficult not only due to the rarity of this type of tumor but also due to the patient’s history of brain meningioma. In August 2019, the patient underwent a craniotomy to remove a meningioma. This explains why the possibility of the post-operative spinal seeding of epidural meningioma could not be ruled out. After admission, MRI imaging showed a hyperintense mass in both T2 ( Fig. 1A) and T1 ( Fig. 1B) imaging at the T11 and T12 levels. It also showed homogenous enhancement in T1-contrast enhanced image ( Fig. 1C). The mass was compressing the cord at that level and had spread to the neural foramina. Based on the patient’s history and the MRI imaging findings, we suspected an epidural meningioma. We carried out surgical tumor removal. Pedicle screws were inserted at the T11-T12 level. Laminectomy and facetectomy were done. An Encapsulated mass with easily identifiable margins was exposed and removed. Postoperative MRI confirmed that the mass was completely removed ( Fig. 2). Pathology revealed adipocytes with abundant vasculature, making the final diagnosis SAL ( Fig. 3). The patient recovered well. His preoperative myelopathy symptoms were gradually relieved. In June 2023, approximately five months after surgery, the patient visited an outpatient clinic. Symptoms he complained of before the surgery, such as gait disturbance, motor weakness, and numbness in both feet, had disappeared.
DISCUSSION
SAL was first reported 1890 by Berenbruch and was defined as ‘spinal angiolipoma’ in 1961 by Howard and Helwig 6,13,25,35,39). Benvenutti-Regato et al. 5) reported that there were 178 cases of SAL up to 2015. We found 51 more reported cases ( Table 1) since 2016, making a total of 229 reported cases. Of the 51 cases, 31 were reported at the thoracic level, 13 at the lumbar level, one at the sacral level, four at the thoracolumbar level, and two at the lumbosacral level. According to Rkhami et al. 30), 78% of SALs are found at the thoracic level, followed by 10% at the lumbar level and, less than 1% at the cervical or sacral level. The tumor is commonly found in the posterior cord at thoracic levels. The symptoms are related to the compression of the thoracic spinal cord 31,40). Common symptoms include lower limb weakness, sensory changes, and numbness 31,40). Symptom progression can vary widely among patients, ranging from simple back pain to acute paraplegia 18,31,40). According to Josephs et al. 17), several factors related to the growth of SAL are trauma, weight gain, and hormones 30). Obesity and pregnancy can promote SAL growth by stimulating hormones that affect the growth of adipose tissue 4,9,23,25,28,31,38). Differential diagnoses of SAL include arteriovenous malformations, nerve sheath tumors, meningioma, metastasis, chronic extradural hematoma, and lymphoma 4,12,24,25,29). Among them, the growth patterns of spinal epidural meningiomas are commonly the en plaque, dumbbell or fusiform type 24,44). The mass may extend toward the intervertebral foramen with a characteristic dura tail 24,44). Out of the three common shapes, the fusiform-shaped meningioma must be differentiated from SAL 24,44). Our patient’s imaging study revealed a mass at the thoracic level. The shape was fusiform with slight dural thickening extending to the intervertebral foramen ( Fig. 1). Based on the imaging study and the patient's history of meningioma, we preoperatively suspected a case of spinal meningioma. MRI is the most valuable tool for diagnosing SAL before surgery 1,4,19,23,27,38,46). Though tumors display variable intensity across T1 and T2, they are usually hyperintense in both T1 and T2-, and homogenously enhanced in T1 images 1,8,18,29,30,38,39). However, in SAL cases with profuse vasculature, T1 displays hypointensity and T2 displays hyperintensity 39,41,42,46). SAL can be subdivided into two types. The first is the non-infiltration type. This subtype is more common and is commonly found within the dorsal epidural space; it is encapsulated, distinguishing it from the surrounding tissue 1,28,32,38,42). Therefore, this type can be completely removed 1,18,28,32,33,35,38,42,46). The second type is the infiltration type, which is less common. This type is commonly found on the ventral side of the spinal cord. It is difficult to distinguish from the surrounding tissue. It usually invades the vertebral body because it is not encapsulated 1,18,28,32,33,35,38,42,46). SAL usually shows a good prognosis with no additional treatments needed, even when the tumor is subtotally removed 1,4,12,16,18,21,27,29,31,46). However, Wang and Tang 39) reported that myelopathy can recur in cases of incomplete removal due to dura infiltration. Total resection is the treatment of choice. Most patients of surgically removed SAL are relieved of neurologic symptoms 1,4,8,18,19,21,22,42,43). The choice of surgical method depends on the tumor’s axial localization (ventral or dorsal) and the involvement of the intervertebral foramen 45). The tumor is usually located dorsally without involvement of the intervertebral foramen 1,28,32,38,42). In such cases, total resection is relatively easy without dura injury 45). However, in cases of a ventral location with the involvement of the intervertebral foramen, wider resection is necessary 45). In our case, the wide resection method with laminectomy and facetectomy was selected, as the tumor was located dorsally-, but invaded the intervertebral foramen. After removal of the tumor, screw fixation was performed for spine stability. Pathologically, SAL shows a characteristic appearance of mature adipocytes and abnormal vascular elements, including capillaries, thin- or thick-walled vessels, and small arteries 4,20,37,39,42,46). Furthermore, mature fat tissue and blood vessels usually exist at 1:3 to 2:3 39).
CONCLUSION
SAL is a rare benign tumor composed of fat tissue and vasculature. The case reported here was the non-infiltration type with a clear margin. After the tumor was completely removed, the patient was discharged with improved myelopathy symptoms. Treatment for SAL involves surgical resection. The prognosis is good after surgery.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgments
This work was supported by a grant of Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and future planning (RS-2023-00209591).
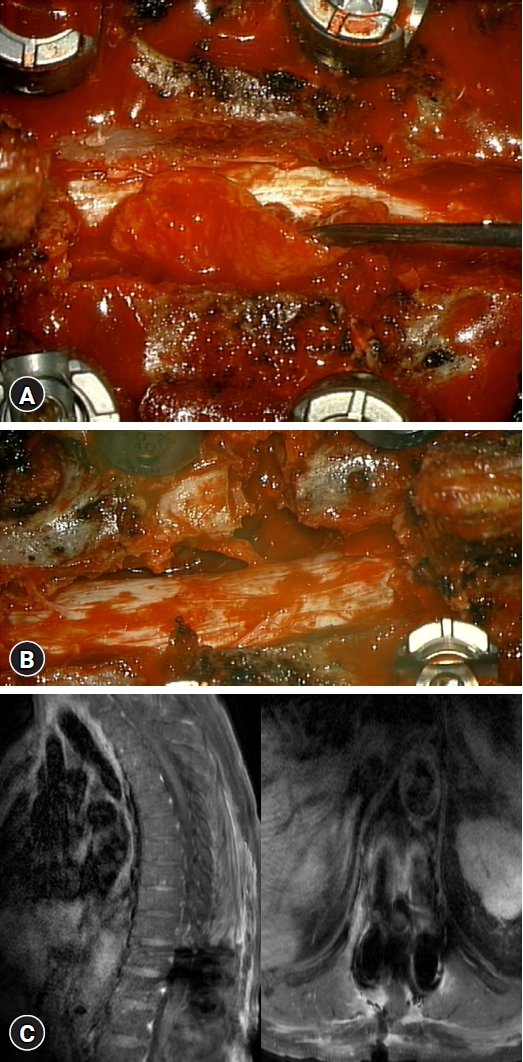
Fig. 1.
(A) T2-weighted magnetic resonance imaging (MRI) showing a hyperintense mass at T11-12. (B) T1-weighted MRI showing a hyperintense mass at T11-12. (C) Post-contrast T1-weighted MRI showing a well-enhanced mass compressing the spinal cord and spreading to the neural foramina at T11-12. 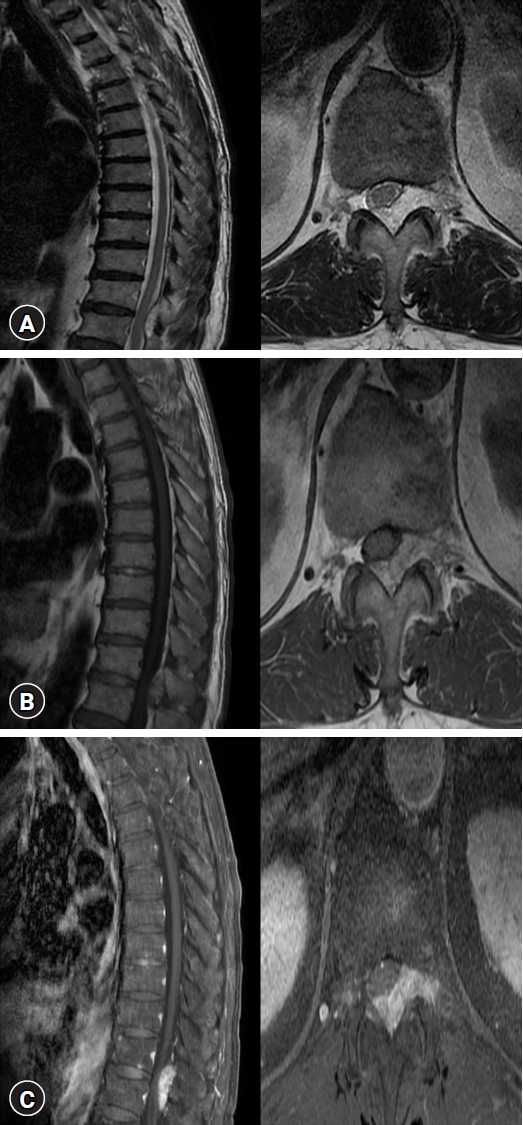
Fig. 2.
(A) Intraoperative picture showing a yellow mass on the dura at T11-12. (B) Complete removal of the mass through laminectomy and facetectomy. (C) Complete removal of the mass on postoperative magnetic resonance imaging. 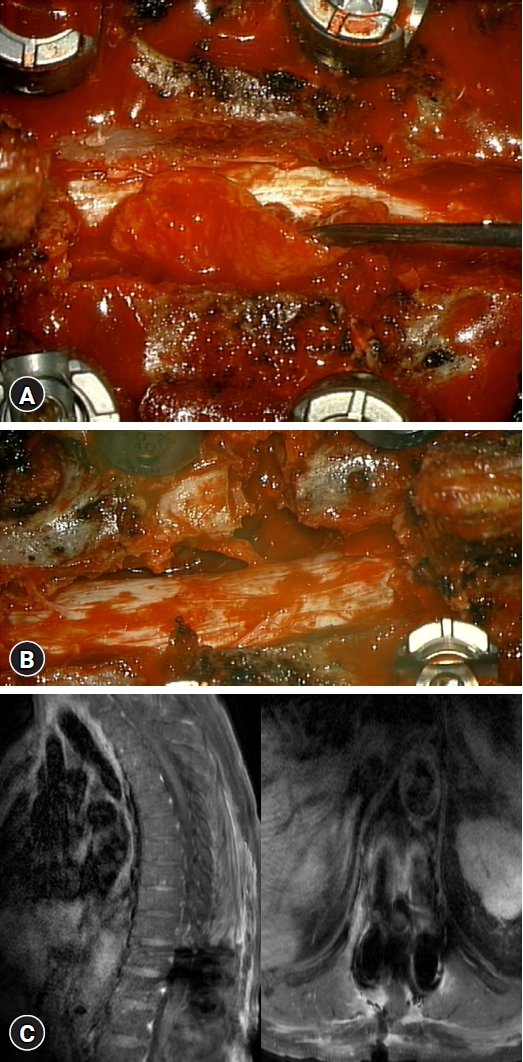
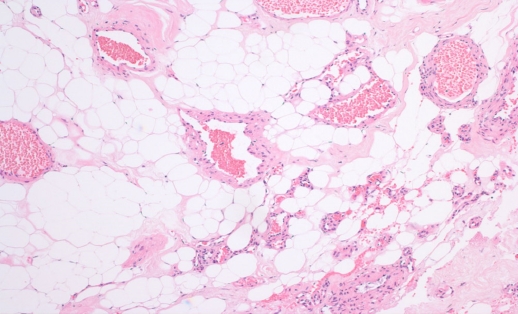
Fig. 3.
Histopathological image (hematoxylin and eosin stain) showing mature adipocytes with extensive vasculature. 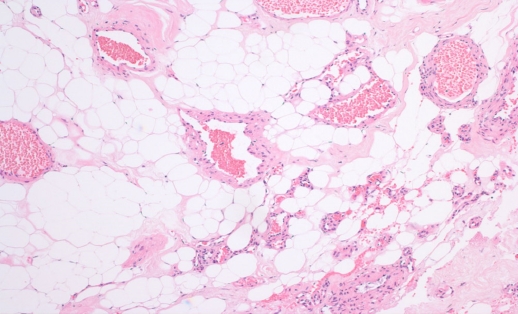
Table 1.
Review of reported cases of spinal angiolipoma since 2016
|
No. |
References |
Year |
Sex/Age |
Level |
Signs |
Treatment |
|
1 |
Sim et al. 32)
|
2016 |
F/58 |
T2-6 |
Thoracic back pain |
Surgery |
|
2 |
F/42 |
T11-L2 |
Numbness of legs |
Surgery |
|
3 |
M/39 |
T3-6 |
Ascending numbness |
Surgery |
|
4 |
F/26 |
L5-S1 |
Gait disturbance |
Surgery |
|
5 |
Mohammed and Ahmed 28)
|
2016 |
F/35 |
T5-8 |
Lower limb paralysis |
Surgery |
|
6 |
Glynn et al. 9)
|
2016 |
F/37 |
T6-9 |
Weakness of the lower limbs |
Surgery |
|
7 |
Isla et al. 16)
|
2016 |
F/69 |
L1-2 |
Lower back pain |
Surgery |
|
8 |
Ying et al. 43)
|
2017 |
M/63 |
L2-3 |
Lower back pain |
Endoscopic Surgery |
|
9 |
Onishi et al. 29)
|
2017 |
F/35 |
T3-5 |
Paraparesis |
Surgery |
|
10 |
Wang et al. 38)
|
2017 |
F/25 |
L3-4 |
Lower back pain |
Surgery |
|
11 |
F/77 |
T2-4 |
Numbness of legs |
Surgery |
|
12 |
F/45 |
T4-6 |
Numbness of legs |
Surgery |
|
13 |
Mohammed et al. 27)
|
2017 |
M/68 |
T5-7 |
Weakness of the lower limbs |
Surgery |
|
14 |
Kang et al. 18)
|
2017 |
M/69 |
L2-3 |
Numbness of legs |
Surgery |
|
15 |
Akyuva et al. 1)
|
2017 |
F/65 |
L2-3 |
Left leg weakness |
Surgery |
|
16 |
Shweikeh et al. 31)
|
2017 |
M/55 |
T3-8 |
Back pain, radiating pain to scapula |
Surgery |
|
17 |
Tseng et al. 35)
|
2017 |
F/48 |
L1-2 |
Lower back pain |
Surgery |
|
18 |
Wani et al. 40)
|
2018 |
M/60 |
T6-7 |
Weakness of the lower limbs |
Surgery |
|
19 |
Rkhami et al. 30)
|
2018 |
F/65 |
T7-10 |
Weakness of the lower limbs |
Surgery |
|
20 |
Tateiwa et al. 34)
|
2018 |
M/76 |
L2-4 |
Left lower radiculopathy |
Surgery |
|
21 |
Yang et al. 42)
|
2018 |
F/39 |
T5-7 |
Numbness of legs |
Surgery |
|
22 |
M/53 |
T12-L1 |
Right leg pain |
Surgery |
|
23 |
Horiuchi et al. 12)
|
2018 |
F/49 |
T5-8 |
Weakness of the lower limbs |
Surgery |
|
24 |
Lacour et al. 21)
|
2018 |
M/17 |
T7-12 |
Paraplegia |
Surgery |
|
25 |
Maduri et al. 25)
|
2019 |
F/29 |
T5-9 |
Weakness of the lower limbs |
Surgery |
|
26 |
Khelifa et al. 19)
|
2019 |
F/26 |
T2-4 |
Weakness of the lower limbs |
Surgery |
|
27 |
Krishnan 20)
|
2019 |
M/20 |
L2-3 |
Lower back pain |
Surgery |
|
28 |
Zhang et al. 46)
|
2020 |
F/54 |
T4-6 |
Back pain |
Surgery |
|
29 |
Ikpeze et al. 15)
|
2020 |
F/39 |
L1-2 |
Lower back pain |
Surgery |
|
30 |
Wang and Tang 39)
|
2020 |
F/47 |
L1-2 |
Lower back pain |
Surgery |
|
31 |
M/61 |
T5-7 |
Lower back pain |
Surgery |
|
32 |
Apostolakis et al. 2)
|
2020 |
M/35 |
T7-9 |
Gait disturbance |
Surgery |
|
33 |
M/46 |
T11-L1 |
Lower back pain |
Surgery |
|
34 |
Cheng et al. 8)
|
2020 |
M/54 |
T3 |
Numbness below the nipple |
Surgery |
|
35 |
Gupta et al. 11)
|
2020 |
F/55 |
T11-L1 |
Tingling sensation of lower limbs |
Surgery |
|
36 |
Canbek et al. 7)
|
2020 |
F33 |
T11-12 |
Back pain |
Surgery |
|
37 |
Iampreechakul et al. 14)
|
2020 |
F/55 |
S3-4 |
Paraparesis |
Surgery |
|
38 |
Benhayoun et al. 4)
|
2021 |
M/35 |
T7-10 |
Paraplegia |
Surgery |
|
39 |
Mallard et al. 26)
|
2021 |
F/51 |
L2-4 |
Lower back pain |
Surgery |
|
40 |
Lee et al. 23)
|
2021 |
M/60 |
T3-5 |
Gait disturbance |
Surgery |
|
41 |
Velayudhan et al. 36)
|
2021 |
F/76 |
T6 |
Paraplegia |
Surgery |
|
42 |
Gulnarakhon et al. 10)
|
2021 |
F/63 |
T9-11 |
Lower back pain |
Surgery |
|
43 |
F/40 |
L2-3 |
Left leg radiating pain |
Surgery |
|
44 |
Bachir et al. 3)
|
2022 |
F/26 |
T2-4 |
Weakness of the lower limbs |
Surgery |
|
45 |
Liu et al. 24)
|
2022 |
F/66 |
T7-9 |
Weakness of the lower limbs |
Surgery |
|
46 |
Vijayan et al. 37)
|
2022 |
M/61 |
T6-9 |
Lower back pain |
Surgery |
|
47 |
Laeke et al. 22)
|
2022 |
M/47 |
T1-2 |
Lower legs weakness |
Surgery |
|
48 |
Somrani et al. 33)
|
2022 |
F/54 |
L5-S1 |
Right lumbosciatica |
Surgery |
|
49 |
Josephs et al. 17)
|
2022 |
F/59 |
L2-3 |
Lower back pain |
Surgery |
|
50 |
Xu et al. 41)
|
2023 |
F/42 |
T4-7 |
Weakness of the lower limbs |
Surgery |
|
51 |
This case |
2023 |
M/81 |
T11-12 |
Gait disturbance |
Surgery |
|
|
|
|
|
|
|
REFERENCES
2. Apostolakis S, Karagianni A, Mitropoulos A, Mantas C, Mavridis I, Filias P, et al.: Spinal angiolipoma: Presentation of two cases and review of the literature for the years 2012-2017. Neurocirugia (Astur : Engl Ed) 31:76-86, 2020   3. Bachir S, Aoudia D, Baki N, Daou D, Lahbib A: Spinal epidural angiolipoma causing spinal cord compression. A case report. Avicenna Med Res 1:44-46, 2022
4. Benhayoun O, Makhchoune M, Jehri A, Yassine Haouas M, Hilmani S, Lakhdar A: Spinal extradural angiolipomas: A case report. Ann Med Surg (Lond) 65:102289, 2021  6. Berenbruch K: Ein fall von multiplen angiolipomen kombiniert mit eniem angiom des ruckenmarks. Tübingen, DE: Lupp, 1890. Berenbruch K. Ein fall von multiplen angiolipomen kombiniert mit eniem angiom des ruckenmarks. Tübingen, DE: Lupp, 1890
7. Canbek I, Vural S, Ak H: Incidental thoracic spinal angiolipoma in a young woman presenting with trauma. J Emerg Med Case Rep 11:79-81, 2020  8. Cheng Y, Lu K, Jiang H: Epidural angiolipoma with concomitant intradural extramedullary capillary hemangioma at the same spinal level: A case report. Oncol Lett 20:209-214, 2020  9. Glynn D, Murray B, Cryan J, O'Brien D, Kavanagh E: Spinal epidural angiolipoma. Spine J 16:e531-e532, 2016  10. Gulnarakhon A, Khusniya G, Jasur S, Khabibullo K: Spinal extradural angiolipomas. Case report and literature review. Sci Time 9:29-34, 2021
11. Gupta SK, Chhabra A, Prajapati HK, Ahmad F: Dorsolumbar angiolipoma. A rare case report and review of literature. Rom Neurosurg 34:540-543, 2020  12. Horiuchi K, Yamada T, Sakai K, Okawa A, Arai Y: Hemorrhagic sudden onset of spinal epidural angiolipoma. Case Rep Orthop 2018:5231931, 2018   13. Howard WR, Helwig EB: Angiolipoma. Arch Dermatol 82:924-931, 1960   14. Iampreechakul P, Tangviriyapaiboon T, Liengudom A, Lertbutsayanukul P, Thammachantha S, Siriwimonmas S: Sacral extradural angiolipoma associated with tight filum terminale and spina bifida coexisting with spinal arteriovenous fistula. World Neurosurg 140:37-45, 2020   15. Ikpeze T, Kulp A, Williams D, Huber A, Mesfin A: Lumbar extradural angiolipoma: Clinical presentation and management. Cureus 12:e12380. 2020  16. Isla A, Ortega Martinez R, Pérez López C, Gómez de la Riva A, Mansilla B: Lumbar spinal angiolipoma. Neurocirugia (Astur) 27:258-262, 2016   17. Josephs M, Selph J, Funk C, Lubert J, Walker A, Green D, et al.: Epidural angiolipoma presenting with spinal cord compression: Case report and review of the literature. MOH J Med Case Rep 1:46-49, 2022
19. Khelifa A, Assoumane I, Bachir S, Berchiche L, Morsli A: Spinal epidural angiolipoma causing spinal cord compression: A case report. Rom Neurosurg 33:326-328, 2019
20. Krishnan RK: Spinal angiolipoma in the lumbar region-a rare case report. Univ J Surg Surg Spec 5:2019
21. Lacour M, Gilard V, Marguet F, Curey S, Perez A, Derrey S: Sudden paraplegia due to spontaneous bleeding in a thoracic epidural angiolipoma and literature review. Neurochirurgie 64:73-75, 2018   22. Laeke T, Yibeltal M, Kwon YD: Thoracic spinal angiomyolipoma: Case report from an Ethiopian neurosurgical teaching hospital. Illustrative case. J Neurosurg Case Lessons 4:CASE22216, 2022  23. Lee CH, Son DW, Lee SH, Lee JS, Lee SW, Song GS: Spinal epidural angiolipoma: A case report on sudden hemorrhagic onset and review of the literature. J Korean Soc Geriatr Neurosurg 17:20-24, 2021   25. Maduri R, Belouaer A, Brouland JP, Ecker T, Messerer M: Spinal angiolipomas in pregnancy: Natural history and surgical treatment. Clin Neurol Neurosurg 178:25-30, 2019   26. Mallard F, Buni M, Nolet PS, Emary P, Taylor JA, Moammer G: Lumbar spinal epidural lipomatosis: A case report and review of the literature. Int J Surg Case Rep 78:71-75, 2021   32. Sim K, Tsui A, Paldor I, Kaye AH, Gaillard F: Four cases of spinal epidural angiolipoma. J Clin Neurosci 25:134-139, 2016   35. Tseng SC, Hsieh CT, Chang CJ: Lumbar epidural angiolipoma: A rare case report. Fu Jen J Med 15:203-208, 2017
37. Vijayan SP, Gerber C, Basu A, Basu G, Mhatre R: Epidural angiolipoma and andersson lesion: A rare co-occurence - A case report and literature review. Indian Spine J 5:235-240, 2022  39. Wang R, Tang H: Spinal angiolipoma: a report of two cases and review of the literature. J Int Med Res 48:300060520954690, 2020   43. Ying GY, Yao Y, Shen F, Ren YC, Chen CM, Zhu YJ: Percutaneous endoscopic removal of a lumbar epidural angiolipoma via interlaminar approach: A technical report. World Neurosurg 99:59-62, 2017   46. Zhang X, Wang JJ, Guo Y, Dong S, Shi W, Wang G, et al.: Sudden aggravated radicular pain caused by hemorrhagic spinal angiolipomas after back massage. World Neurosurg 134:383-387, 2020  
|
|