AbstractThe surgical treatment of spondylitis involves potential risks, especially when dealing with infected tissues that may be fragile and susceptible to injury from surgical trauma and inflammation. In cases where spondylitis is not controlled even after the initial surgery, unexpected situations can arise if an unusual change in infected tissues around the spine is misinterpreted. The present case involves a 62-year-old who underwent laminectomy, debridement, and stabilization from T12 to L2 due to medically intractable spondylitis caused by methicillin-resistant Staphylococcus aureus. No major bleeding or vascular injury occurred during surgery. However, despite some improvement in pain and weakness, inflammation markers remained elevated and back pain recurred. A computed tomography (CT) scan taken 15 days after surgery showed a round-enhancing lesion inside the L1 vertebra. Although the primary imaging diagnosis suggested a loculated abscess, a round-enhancing lesion raised suspicion of an unusual pseudoaneurysm. A CT angiography confirmed a pseudoaneurysm from the L1 segmental artery, successfully treated with endovascular embolization. After embolization, the patient’s back pain improved, and inflammation markers further decreased with oral antibiotics. This case highlights the possibility of a pseudoaneurysm occurring in cases of spondylitis, emphasizing the importance of considering this entity in the differential diagnosis to ensure proper treatment.
INTRODUCTIONThe primary treatment for spondylitis involves medical interventions, and surgery becomes necessary if medical treatment proves ineffective. The decision to proceed with surgery is based on clinical symptoms, laboratory findings, and imaging studies. Surgery is recommended when these results indicate that the infection is not under control4,6,8,11). Surgical procedures include laminectomy, drainage of abscess, debridement and culture of infected tissue1,4). Spinal instrumentation is performed for several objectives, such as controlling pain, restoring spinal vertebral height, correcting deformity and facilitating early ambulation. These surgical procedures are commonly employed in typical spinal surgeries. However, it is essential to be cautious, as surgical trauma and the inflammatory process can potentially cause damage to infected fragile tissues, including blood vessels19). A secondary surgery is not uncommon when spondylitis is not effectively controlled even after the first surgery. However, unexpected situations can arise if healthcare providers fail to consider unusual changes in the infected tissues surrounding the affected area. It is crucial to carefully assess the patient’s condition and monitor the response to treatment to avoid potential complications and ensure appropriate management2).
The main cause of intravertebral pseudoaneurysm is trauma, but local infection, such as spondylitis or iatrogenic trauma can also lead to the development of intravertebral pseudoaneurysm12,15,18,20). The interpretation of imaging studies for spinal infection is not simple and a paradoxical change occurred despite improved clinical and laboratory findings3,5). Therefore, a prudent interpretation is required for spinal infection, especially when a surgical treatment is considered. We experience a patient with spondylitis and a newly developed intravertebral enhancing round lesion.
CASE REPORTA 62-years-old man had back pain (numerical rating pain scale [NRS] 5/10) and weakness (manual motor grade IV+/V on both legs) on both legs for 2 weeks due to lumbar spondylitis and bilateral psoas abscess by Methicillin-Resistant Staphylococcus aureus infection. He had underlying diabetes and end-stage renal disease requiring regular hemodialysis for more than 10 years. Medical treatment included vancomycin (10 mg/kg) and percutaneous drainage of the abscess. Medical treatment until hospital day 8, but laboratory findings showed that the infection was not medically controlled. Percutaneous drainage of the abscess was not effective. Although the assessment of the effectiveness of antibiotic treatment is limited due to its short duration, considering the patient’s symptoms, a surgical treatment plan was devised in conjunction with antibiotic therapy (Fig. 1).
He was consulted for surgical treatment. Upon physical examinations, the patient had severe tenderness on back (NRS 7/10) and weakness on both legs (manual motor grade IV-/V on both legs). He was underwent surgical treatment at the hospital on day 9. Preoperative imaging studies including magnetic resonance imaging and computed tomography scan (CT) showed spondylitis at L1, epidural abscess and abscesses in bilateral psoas (Fig. 2). Laminectomy, removal of infected epidural tissue, debridement of infected tissue inside of L1 vertebra and instrumentation from T12-L2 were performed. After surgery, vancomycin was continued, and pain and laboratory findings showed improved spondylitis with time. However, the inflammatory makers in blood were not normalized and the patient complained of relapse of back pain (NRS 10/10)
A follow-up CT scan conducted 15 days after the surgery revealed reduced abscess size in the psoas and epidural space. However, a new round-enhancing lesion was observed inside of L1 vertebra (Fig. 3A, B). The initial imaging diagnosis indicated a loculated abscess and surgery was considered a treatment option. However, a distinct, well-defined, round-shaped enhancing lesion also suggested a vascular lesion. Upon further discussion with the physician and radiologist, a pseudoaneurysm was included in the list of differential diagnosis. CT angiogram scan revealed it was a pseudoaneurysm. The pseudoaneurysm was treatment with embolization. A CT angiography revealed a pseudoaneurysm arisen from L1 segmental artery and the aneurysm was embolized with a coil on hospital day 31 (Fig. 4A, B). The back pain was improved to a tolerable level (NRS 5/10) after embolization and infection markers were decreased with continued intravenous antibiotics with adjunctive rifampin. The patient was discharged with oral suppressive antibiotics after 10 weeks of intravenous antibiotic treatment with improved back pain and leg weakness on hospital day 36 days.
DISCUSSIONWe reported a non-traumatic intravertebral pseudoaneurysm that developed in a patient with spondylitis. The exact mechanism of pseudoaneurysm formation is not clear, but it is speculated to occur due to direct surgical trauma to the segment artery or by weakening of arterial wall due to infection9,18,20). The causes of lumbar artery pseudoaneurysm were mostly direct injury to the artery such as blunt trauma, gunshot, stab injury, bleeding disorders, vertebral fracture and iatrogenic trauma such as complication of vertebral biopsy, lumbar disc surgery, and laparoscopic surgery16,17,19). A pseudoaneurysm can develop even without a direct vascular injury during surgery, owing to potential harm to the blood vessels surrounding the surgical area10,14). However, indirect injury after inflammatory process was not uncommon after infection7). In this case, the round lesion in L1 vertebra did not present before surgery and appeared after the first surgery. We did not think that a direct injury of arterial wall caused the pseudoaneurysm because arterial bleeding did not occur during the debridement of infected tissue inside L1 vertebra at the initial surgery and cortical bone of L1 vertebra was not violated. Although the exact cause of the current case was not clear, weakening of arterial wall by infection and inflammation and formation of dead space by restoration of the height of L1 vertebra and debridement of infected tissue inside of L1 vertebra, may have caused pseudoaneurysm7). If a surgical debridement was tried for the round-enhancing “abscess like” lesion, uncontrolled bleeding may have occurred during surgery. Although formation of pseudoaneurysm with spondylitis was rare, a high suspicion of pseudoaneurysm was important for proper treatment7). The treatments available for pseudoaneurysm were endovascular embolization and surgical excision. Between these two options, endovascular embolization was recommended as a primary choice due to surgical difficulties and fatal complications, such as uncontrollable intraoperative arterial bleeding13,19). In this case, we treated the pseudoaneurysm with endovascular embolization without any complications and we treated spondylitis with antibiotics.
CONCLUSIONAlthough the interpretation of imaging studies for spinal infection is challenging, consideration of potential life-threatening pathology should be included in the differential diagnosis. A pseudoaneurysm can develop after spondylitis and it should be considered in the differential diagnosis when a clearly margined round-enhancing lesion is observed in the vertebral body. Endovascular intervention can effectively treat the pseudoaneurysm without risk of surgical complications.
NotesFUNDING This study was supported by grant no. 30-2023-0120 from Seoul National University Hospital research fund. This study was supported by Doosan Yonkang foundation (800-20210527). There was no additional external funding received for this study. Fig. 1.Graph showing changes in inflammatory markers during the patient’s hospital stay. Day 9 was the time of initial surgery. The time of pseudoaneurysm detection (arrow) and embolization (arrowhead) are marked in the graph. WBC: white blood cell; CRP: C-reactive protein; OP: operation; ESR: erythrocyte sedimentation rate. 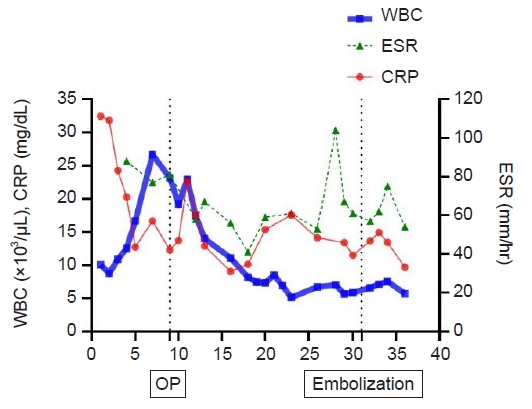
Fig. 2.Preoperative computed tomography (CT) scan. A coronal enhanced CT scan shows spondylitis with an abscess formed along both psoas muscles (large arrows). A percutaneous drain is located in the left psoas muscle abscess (small arrow). There is no enhancing lesion inside the L1 vertebra (black arrow). 
REFERENCES1. Abramovitz JN, Batson RA, Yablon JS: Vertebral osteomyelitis. The surgical management of neurologic complications. Spine (Phila Pa 1976) 11:418-420, 1986
2. Acosta FL, Chin CT, Quiñones-Hinojosa A, Ames CP, Weinstein PR, Chou D: Diagnosis and management of adult pyogenic osteomyelitis of the cervical spine. Neurosurg Focus 17:E2, 2004
3. Brant-Zawadzki M, Burke VD, Jeffrey RB: CT in the evaluation of spine infection. Spine (Phila Pa 1976) 8:358-364, 1983
4. Chen LH, Fu TS, Kao YH, Tsai TT, Lai PL, Niu CC, et al.: Surgical treatment of infectious spondylitis in patients undergoing hemodialysis therapy. Eur Spine J 19:2223-2228, 2010
5. Chianca V, Chalian M, Harder D, Del Grande F: Imaging of Spine Infections. Semin Musculoskelet Radiol 26:387-395, 2022
6. Dimar JR, Carreon LY, Glassman SD, Campbell MJ, Hartman MJ, Johnson JR: Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine (Phila Pa 1976) 29:326-332, 2004
7. Heianna J, Miyauchi T, Takano Y, Hashimoto M, Watarai J: Successful treatment of a ruptured infected aneurysm of the lumbar artery with transcatheter embolization. Abdom Imaging 30:270-273, 2005
8. Kim SS, Kang DH, Yoon JW, Park H, Lee CH, Hwang SH: Surgical treatment of pyogenic spondylitis with the use of freeze-dried structural allograft. Korean J Spine 11:136-144, 2014
9. Koenigsberg AD, Solomon GD, Kosmorsky G: Psuedoaneurysm within the cavernous sinus presenting as cluster headache. Headache 34:111-113, 1994
10. Kutay V, Harman M, Ekim H, Yakut C: Chronic pseudoaneurysm of the aortic arch: a case report. J Card Surg 20:542-544, 2005
11. Larson SJ, Holst RA, Hemmy DC, Sances A: Lateral extracavitary approach to traumatic lesions of the thoracic and lumbar spine. J Neurosurg 45:628-37, 1976
12. Maleux G, Vermylen J, Wilms G: Lumbar artery pseudoaneurysm and arteriovenous fistula as a complication of laparoscopic splenectomy: treatment by transcatheter embolization. Eur Radiol 12:1401-1404, 2002
13. Marty B, Sanchez LA, Wain RA, Ohki T, Marin ML, Bakal C, et al.: Endovascular treatment of a ruptured lumbar artery aneurysm: case report and review of the literature. Ann Vasc Surg 12:379-383, 1998
14. Mosquera VX, Velasco C, Gulias D, Fariña MM: Traumatic brachiocephalic trunk pseudoaneurysm. J Card Surg 28:430-432, 2013
15. Papadoulas S, Konstantinou D, Kourea HP, Kritikos N, Haftouras N, Tsolakis JA: Vascular injury complicating lumbar disc surgery. A systematic review. Eur J Vasc Endovasc Surg 24:189-195, 2002
16. Sclafani SJ, Florence LO, Phillips TF, Scalea TM, Glanz S, Goldstein AS, et al.: Lumbar arterial injury: Radiologic diagnosis and management. Radiology 165:709-714, 1987
17. Shigematsu Y, Kudoh K, Nakasone Y, Fujisaki T, Uemura S, Yamashita Y: Nontraumatic rupture of lumbar artery causing an intravertebral body pseudoaneurysm: treatment by transcatheter embolization. Cardiovasc Intervent Radiol 29:870-874, 2006
18. Silberzweig JE: Ruptured lumbar artery pseudoaneurysm: a diagnostic dilemma in retroperitoneal hemorrhage after abdominal trauma. J Trauma 46:531-532, 1999
|
|
|||||||||||||||||||||||||||||||||||||