INTRODUCTION
Severe cord compression due to soft disc herniation of the cervical spine may have slowly progressive myelopathic symptoms such as paresthesia, dysesthesia, or motor weakness, but in uncommon cases, acute quadriplegia may occur. Sudden, non-traumatic cervical disc herniations presented with acute paralysis of the limbs have been rarely reported and had poor prognosis2-4,6,7,9,11). Irreversible damage can result from injury of the spinal cord to a narrowed spinal canal, reduced blood supply and failure of autoregulation5,8). It is thought that decompression before symptoms and irreversible damage to the cord will help improve the patient's symptoms. We present two uncommon cases of acute paralysis of the limbs due to non-traumatic cervical disc herniation.
CASE REPORT
Case 1
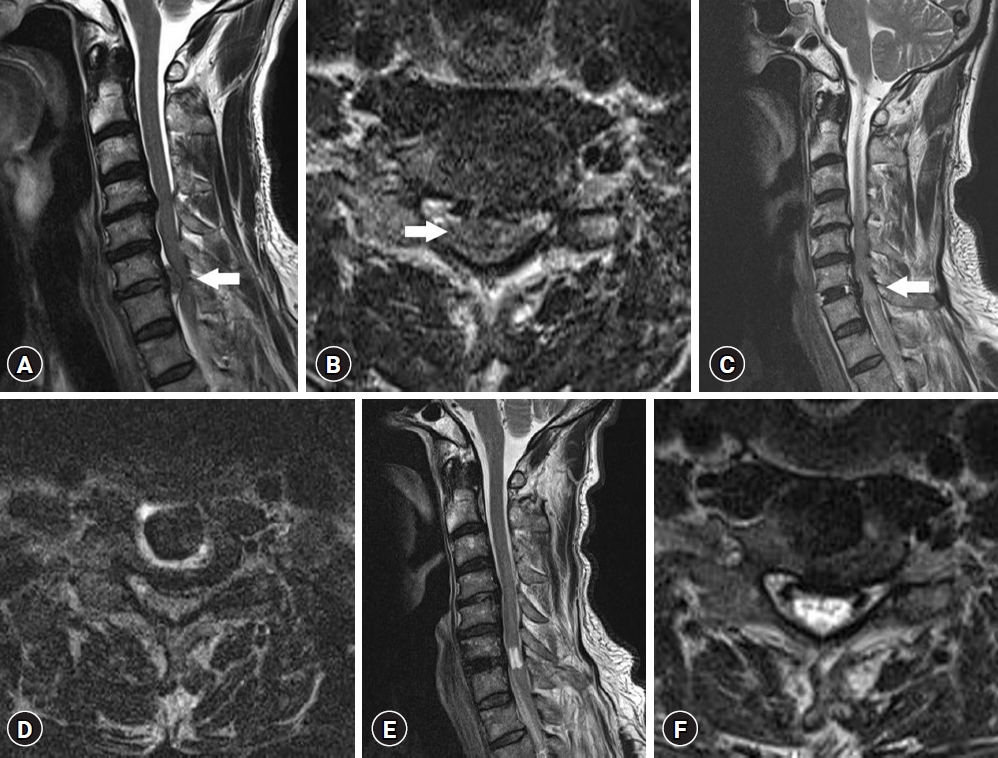
A 61-year-old man presented with sudden quadriplegia 2 hr ago before the patient visited our hospital. He had no specific medical history and was healthy. On admission, vital signs were stable. Initial neurological examinations showed alert mentality, motor weakness of grade 3 of both elbows, wrists, and fingers and grade 0 of both lower limbs, hypesthesia below the T2 level, voiding difficulty and complete loss of anal tone. Additionally, Hoffmann's sign was positive and the deep tendon reflex (DTR) of the limbs was hyperactive. Initial computed tomography of the brain showed normal findings. We suspected the lesion of the cervical spine for quadriparesis. Magnetic resonance imaging (MRI) of the cervical spine revealed huge, soft central disc herniation at the C6-7 level, which had severe cord compression (Fig. 1A, B). At admission, the modified Japanese Orthopaedic Association (mJOA) score was 5.
After about 10 hr of the onset of symptoms, emergent anterior cervical microdiscectomy and fusion were performed at the C6-7 level. During surgery, disc extrusion with craniocaudal migration and severe cord compression due to disc herniation were observed. After decompression, the operation was completed with insertion of a polyetheretherketone (PEEK) cage (SHIVAS® cage 6/14 mm; Seohan Care, Gimpo, Korea) with demineralized bone matrix (DBM; EDENFUSE®; CGBio Inc., Seongnam, Korea). Postoperative mJOA score improved to 8. The postoperative course was uneventful. At postoperative 2-day, the patient was able to lift his shoulder and recovered enough to lift a spoon, but both lower limbs showed no improvement. The motor weakness of both elbows and wrists improved to grade 4. MRI of the cervical spine 3 days after surgery showed that the previous herniated disc material was completely removed, but cord signal change of the C6-7 level and diffuse cord edema to the upper thoracic level under the lesion were observed (Fig. 1C, D). Methylprednisolone 125 mg twice a day was infused for 4 days. Diffuse cord edema disappeared completely, but cord signal change of the C6-7 level still remained on MRI of the cervical spine 4 months after surgery (Fig. 1E, F). Afterwards, he was transferred to the department of rehabilitation medicine and received physical therapy. Motor evoked potential and sensory evoked potential 5 months after surgery showed prolongation of both the upper limbs and both lower limbs and motor evoked potential loss of the pudendal nerve was found. Fourteen months after surgery, the motor weakness of both elbows, wrists, and fingers improved to grade 5, but the complete paralysis of both lower limbs and sphincter functions did not improve. The mJOA score was 10.
Case 2
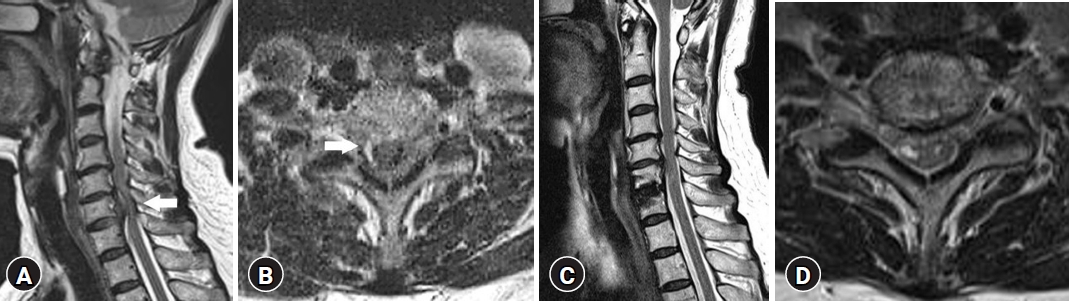
A 65-year-old woman presented with acute right hemiplegia that occurred after waking up 3 hr ago. She had no history of cervical disc disease and also had no history of trauma. She had received manual therapy for neck pain before 1 day. Initial neurological examination, she had alert mentality, right-sided hemiparesis; motor grade 3 of the right elbow, wrist and fingers and motor grade 2 of the right lower limb. Hoffmann's sign was positive and DTR of the right limbs was hyperactive. Urinary function and anal tone were intact. First, diffusion MRI and magnetic resonance angiography of the brain were normal findings. We performed MRI of the spine to exclude the lesion of the spinal cord. MRI of the cervical spine revealed central to right-sided, superior migrated, large disc herniation with severe cord compression and edema at the C6-7 level (Fig. 2A, B). On admission, the mJOA score was 9.
Emergency anterior cervical microdiscectomy and fusion were performed at the C6-7 level after about 9 hr of the onset of symptom. During the operation, the migrated disc material compressing the cord was removed, and a PEEK cage (SHIVAS® cage 7 /14 mm) with DBM EDENFUSE® was inserted. Follow-up MRI of the cervical spine 6 days after surgery showed a tiny cord signal change at the C6-7 level. Just after surgery, her right weakness recovered to grade 4 in the elbow and wrist and grade 3 in the fingers, and the right lower limb of the thigh and knee were grade 3.
DISCUSSION
Our two cases suggest that accurate diagnosis of sudden, non-traumatic soft cervical disc herniation and quick surgery are very important. Non-traumatic, soft cervical disc herniation presented with acute paralysis of the limbs is a very rare surgical entity. Up to date, about ten cases have been reported sporadically in the literature2-4,6,7,9,11). Goh and Li3) reported a case of cervical myelopathy occurring during sleep, related to respiratory insufficiency due to sleep apnea. Liu et al.6) reported a case that the pre-existing narrowed canal and excessive neck movement due to the loss of the lordotic curve of the cervical spine are the causes of quadriplegia due to cervical disc herniation. Some reports have been accompanied by neck pain, motor weakness, and hypesthesia9,11). A herniated disc, when accompanied by cervical canal stenosis can reduce the blood supply to the anterior spinal artery, potentially causing sudden neck pain. It can also result in weakness and hypesthesia9,11). Thus, damage to the spinal cord and reduced blood supply to the narrowed spinal canal results in paralysis and irreversible damage resulting from a sudden soft disc herniation5,8). Decreased blood flow in the anterior spinal artery and branches can lead to permanent cord damage and poor postoperative prognosis5,8).
Some cases report that rapid diagnosis and appropriate surgery before irreversible cord damage can help improve symptoms of sudden quadriplegia4,9,11). Timely surgery with rapid diagnosis is considered the best way to prevent a patient's serious cord injury and avoid postoperative neurologic deficits3,4,6,9,11). The degree of symptomatic recovery depends on the correct diagnosis, emergency surgery, the extent of spinal cord damage, especially irreversible damage. If the herniated disc material compresses the spinal cord, it can lead to neurological deficits that might become irreversible if not treated promptly1,10). Chronic compression of the spinal cord can cause lasting damage to nerve fibers and lead to long-term functional impairments. Factors that can affect irreversible damage include the severity and location of herniation, the time of compression, the size of the spinal canal, the degree of lordosis of the cervical spine, the size of the ruptured disc, and the time until surgery4-6,8,9,11). Emergency surgery due to acute cord compression is controversial, but the patient's prognosis and neurological symptoms are improved when the surgery is performed within 24 to 36 hr1,10).
In diagnosing a patient presented with paralysis of the limbs, mental change seems to be an important difference between brain lesions and spinal cord lesions. First of all, careful neurological examinations should be done to exclude a spinal cord lesion although it is very rare.
In the first case, postoperative MR demonstrated permanent cord damage and the patient’s paralysis of the legs did not improve. It seems to be due to irreversible spinal cord damage caused by severe spinal cord compression in the early stage. However, in the second case, postoperative MR showed decreased cord edema and the patient recovered completely.
Our two cases suggest that surgical decompression should be performed as early as possible to prevent permanent neurological deficit in a patient with non-traumatic, soft cervical disc herniation presented with acute paralysis of the limbs.