AbstractPeripheral neuropathies, including entrapment or injury, are quite common and are encountered frequently. To ensure accurate diagnosis and effective treatment for these conditions, it is essential to have a comprehensive understanding of peripheral nerve anatomy and assessment techniques. This may involve the use of methods like ultrasonography, as well as requiring clinical proficiency. The median nerve, which is one of the main nerves in the upper extremity, primarily controls motor function in the flexor muscles of the forearm and hand. It is responsible for actions such as wrist flexion and the movement of the first three fingers. The purpose of this article is to enhance understanding and improve the diagnosis of peripheral nerve disorders, with a particular focus on neuropathies associated with the median nerve.
INTRODUCTIONPeripheral nerve neuropathies, such as entrapment or injury, are not uncommon and are frequently encountered in outpatient clinics or emergency rooms by medical professionals. Accurate diagnosis and treatment of these conditions require a thorough understanding of peripheral nerve anatomy and assessment methods, including ultrasonography, as well as clinical expertise. In the upper extremity, there are three major nerves - the median, ulnar, and radial nerves. The median nerve primarily provides motor innervation to the flexor muscles of the forearm and hand, controlling wrist flexion and movement of the first three fingers. In contrast, the ulnar nerve innervates a portion of the forearm and the majority of the hand intrinsic muscles, which are crucial for precise and coordinated hand movements. The radial nerve, on the other hand, stimulates the muscles of the posterior arm and forearm, as well as the extrinsic wrist and hand extensors.
The aim of this article is to help readers understand and diagnose peripheral nerve diseases, specifically focusing on median nerve neuropathies. It examines the anatomy of the median nerve and compares its neuropathies to those of other major nerves in the upper extremities.
ANATOMICAL COURSEThe median nerve originates from both the lateral and medial cords of the brachial plexus, receiving contributions from the ventral roots of C6-C7 (via the lateral cord) and C8-T1 (via the medial cord). The lateral cord primarily innervates sensory axons, while the medial cord mainly supplies motor function11). Consequently, the primary motor input comes from the medial cord. As it travels through the upper extremity, such as when it passes between the biceps brachii and triceps brachii muscles, through the antecubital fossa, or down to the wrist, the median nerve consistently stays in a central position (Fig. 1).
1. The ArmAfter receiving inputs from both the lateral and medial cords of the brachial plexus, the median nerve enters the arm through the axilla, passing beneath the lower edge of the teres major muscle. From there, it descends vertically and runs alongside the brachial artery, positioned between the biceps brachii (above) and brachialis (below) (Fig. 2). Initially, it is located at the side of the artery and in front of the shoulder joint. As it continues down the arm and enters the antecubital fossa, it transitions to a position in front of the artery. It should be noted that the median nerve does not innervate any muscles in the arm.
2. The Antecubital FossaIn the antecubital fossa, the median nerve travels medially in relation to the brachial artery. It passes over the brachialis muscle, located medial to the biceps brachii. After that, it branches out to supply the elbow joint and gives off a branch to the pronator teres muscle, located just above the elbow joint5).
As it traverses the antecubital fossa, the median nerve passes beneath three successive arches or tunnels, leading it deep into the forearm: the bicipital aponeurosis (lacertus fibrosis); between the two heads of the pronator teres; and the fibrous arch between the two heads of the flexor digitorum superficialis (FDS), also known as flexor digitorum sublimis11). The first arch it goes under is called the bicipital aponeurosis. This is a thick layer of fascia that connects the biceps brachii to the mass of the proximal forearm. Below this aponeurosis, you'll find the biceps tendon and the brachial artery on the outer side, while the humeral head of the pronator teres muscle is positioned on the inner side in relation to the median nerve11). A short distance beyond the proximal border of the bicipital aponeurosis, the median nerve descends beneath a second structure—the humeral head of the pronator teres muscle. The pronator teres muscle exhibits a Y-shaped configuration, with the lower stem of the Y inserting into the radius distally and laterally. The upper limb of the Y consists of two proximal heads, a larger superficial head attaching to the humerus (humeral head), and a smaller deeper head attaching to the ulna (ulnar head). The median nerve passes through the cleft between these heads, with the ulnar head positioned deep and the humeral head superficial (Fig. 3). It crosses the ulnar artery (branch of brachial artery) while being separated by the deep head of the pronator teres. Just after traversing the pronator teres, the median nerve promptly courses beneath a third anatomical feature: the bifurcated heads of the FDS, forming a Y-shape. Positioned medially is the humeroulnar head, while laterally lies the radial head. Between these heads, a fibrous ridge known as the sublimis bridge is present, and beneath this bridge is where the median nerve travels. Muscular branches are given off in the cubital fossa to supply the flexor carpi radialis (FCR), palmaris longus, and FDS5).
3. The ForearmThe median nerve runs down the middle of the forearm, beneath the FDS but above the underlying flexor digitorum profundus (FDP) muscle (Fig. 4). About halfway down the forearm, the median nerve gives off a significant branch called the anterior interosseous nerve (AIN), which emerges from the dorsolateral aspect. The AIN then travels deeper into the forearm, between the radius and ulna on the interosseous membrane, which is located between the muscle bellies of the FDP and flexor pollicis longus (FPL). Further down the arm, the median nerve resurfaces about 5 cm above the wrist crease, just medial to the FCR tendon. The palmaris longus tendon is located adjacent to the median nerve at the proximal wrist. The AIN supplies innervation to the FPL and the lateral half of the FDP (the ulnar half is supplied by the ulnar nerve, as is the flexor carpi ulnaris [FCU] muscle). It also provides innervation to the pronator quadratus muscle. The palmar cutaneous branch of the median nerve arises from the distal part of the forearm, just before it enters the hand. It provides sensory innervation to the thenar eminence of the palm and the central palm.
4. The Wrist and HandThe median nerve travels through the carpal tunnel, beneath the flexor retinaculum, alongside the nine tendons of FDS, FDP, and FPL (Fig. 5). Once inside the carpal tunnel, the median nerve gives rise to a branch on its radial side known as the recurrent thenar motor branch. As it reaches the deep palm, the median nerve splits into two divisions: the radial and ulnar divisions. The recurrent motor branch supplies the thenar muscles (abductor pollicis brevis [APB], opponens pollicis, and the superficial part of flexor pollicis brevis [FPB]). The radial and ulnar divisions of the median nerve innervate the first and second lumbricals and provide sensory innervation to the radial two-thirds of the palm, as well as the distal volar surface of the first, second, third, and the radial half of the fourth digits through digital branches11).
MOTOR INNERVATION AND ASSESSMENT (Table 1)While the median nerve does not innervate the muscles of the arm, it does have a significant role in innervating several muscles in the forearm and hand. These muscles are involved in forearm pronation, wrist flexion, flexion of the digits (particularly the first three), as well as thumb opposition and abduction (Fig. 6).
1. The Proximal Forearm GroupThis group consists of four muscles: pronator teres, FCR, FDS, and palmaris longus (Fig. 7). The pronator teres (C6, C7) is the main pronator of the forearm and receives innervation from the median nerve. Branches from the median nerve emerge at the lower part of the upper arm and pass between the two heads of the pronator teres. To assess the pronator teres, the patient's forearm is extended and fully pronated, and then the patient is instructed to resist forearm supination by the examiner. The FCR (C6, C7) is one of the major wrist flexors, while the ulnar nerve innervates the FCU, which serves as the other. Testing the FCR involves instructing the patient to flex the wrist in line with the forearm trajectory. The tendon of the FCR can be observed and palpated proximal to the wrist. Palmaris longus (C7, C8) is a small muscle with a tendon located between the FCR and FCU. It acts as a weak wrist flexor and does not provide significant flexing force. Approximately 15% of the population has anatomical variations of palmaris longus, such as its absence. In some cases, the reversed belly of palmaris longus may be found within the carpal tunnel, leading to symptoms of carpal tunnel syndrome (CTS). The FDS (C8, T1) functions as the extrinsic flexor of the second to fifth digits at their proximal interphalangeal joints. To assess the FDS, one finger is flexed at the proximal interphalangeal joint against resistance while the other three fingers are held fully extended to deactivate the FDP (Fig. 8). Each finger is tested individually13).
2. The Anterior Interosseous GroupThis group consists of three anterior forearm muscles located deep within the arm: the FDP (acting on the second and third digits), the FPL, and the pronator quadratus (Fig. 9). The FDP (C8, T1) is innervated by both the median and ulnar nerves. The median nerve controls flexion of the distal interphalangeal joint of the second digit and partially controls the same action in the third digit, while the ulnar nerve regulates this muscle's function in the third (partially), fourth, and fifth digits. To assess the FDP innervated by the median nerve, instruct the patient to flex the distal interphalangeal joint of the second digit against resistance while keeping the metacarpophalangeal and proximal interphalangeal joints immobile (Fig. 10). The FPL (C8, T1) functions as the flexor of the thumb at the interphalangeal joint, similar to the FDP. To evaluate the FPL, direct the patient to flex the distal phalanx of the thumb against resistance while stabilizing the thumb (Fig. 11). A quick method to assess both FDP and FPL innervation from the AIN is to ask the patient to form an "okay" sign by touching the tips of the thumb and index finger together. In cases of weakness affecting both the FDP and FPL due to AIN palsy, the distal phalanges cannot flex, resulting in the fingertips failing to touch and the volar surfaces of each digital phalanx making contact instead. The third muscle supplied by the AIN is the pronator quadratus (C7, C8), which is a weaker forearm pronator compared to the pronator teres. To evaluate the pronator quadratus, instruct the patient to resist supination of the fully flexed and pronated forearm.
3. The Thenar GroupThis group consists of three muscles: APB, FPB, and opponens pollicis. These muscles are innervated by the thenar branch of the median nerve (Fig. 12). The APB (C8, T1) is responsible for thumb abduction, which occurs in two directions: palmar abduction, where the thumb moves away from the palm's plane (controlled by the APB), and radial abduction, where the thumb moves away from the forearm's line (controlled by the abductor pollicis longus, innervated by the radial nerve). To assess the APB, instruct the patient to resist thumb movement away from the palm's plane (palmar abduction), while keeping the metacarpals of the other fingers immobilized (Fig. 13). The FPB (C8, T1) has a superficial head innervated by the median nerve and a deep head innervated by the ulnar nerve. This muscle is responsible for thumb flexion at the metacarpophalangeal joint. To evaluate the FPB, instruct the patient to flex at the metacarpophalangeal joint while immobilizing the thumb's interphalangeal joint (Fig. 14). Use your hand as an examiner to immobilize the first metacarpal to prevent substitution by the opponens pollicis. The opponens pollicis (C8, T1) opposes the thumb and is located deep to the APB and the side of the FPB. To assess the opponens pollicis, instruct the patient to firmly press the volar pads of the distal thumb and fifth digit together, while you attempt to pull the distal first metacarpal away from the fifth digit (Fig. 15).
Although the median nerve is responsible for thumb opposition, it is possible for a combination of thumb adduction (controlled by the ulnar nerve innervated adductor pollicis) and thumb flexion (mediated by the ulnar nerve innervated deep head of the FPB) to mimic thumb opposition in cases where there is complete median nerve palsy. In situations where the median nerve is completely dysfunctional, some thumb movement can still occur due to muscle action from radial and ulnar innervation, or from nearby muscles acting as substitutes.
4. The Terminal GroupThe terminal group consists of the first and second lumbricals (C8, T1). The first lumbrical is innervated by the terminal radial division of the median nerve, while the second lumbrical is innervated by the terminal ulnar division of the median nerve (Fig. 12). The lumbricals are intrinsic muscles of the hand that have two main actions: flexing the metacarpophalangeal joints and extending the interphalangeal joints. They work together with the interosseous muscles to achieve these movements. The third and fourth lumbricals, on the other hand, are innervated by the deep branch of the ulnar nerve. To test the function of the lumbrical, the patient is instructed to extend the index finger at the proximal interphalangeal joint while the finger is stabilized in a hyperextended position at the metacarpophalangeal joint (Fig. 16).
SENSORY INNERVATIONThere are three branches of the median nerve that are responsible for sensory innervation of the hand (Fig. 17). The palmar cutaneous nerve provides innervation to the radial two-thirds of the palm, especially over the thenar eminence. The digital nerves of both the radial and ulnar divisions supply sensation to the distal volar surfaces of the first, second, third, and radial half of the fourth digits. Within the radial division, there is a further division into the common digital nerve for the thumb and the proper digital nerve for the radial half of the index finger. The common digital nerve for the thumb then divides into two proper digital nerves. The ulnar division of the median nerve gives rise to the common digital nerves for the second and third web spaces, which then branch into proper digital nerves. Therefore, during examination, the examiner should use the thenar eminence to assess the palmar cutaneous branch, which passes superficially to the carpal tunnel, and examine the distal portion of the second and third digits to evaluate the sensory fibers that pass through the carpal tunnel.
ENTRAPMENT SYNDROMES1. Pronator syndromeThe median nerve can be trapped at four specific locations around the elbow. It may be compressed at the lower end of the humerus by the ligament of Struthers. Another possible site is at the upper end of the elbow, where the biceps aponeurosis becomes thicker. In addition, compression can occur between the superficial and deep heads of the pronator teres muscle within the elbow joint, which is the most common cause of median nerve compression. Lastly, the nerve can also be compressed at the upper part of the forearm by a thickened proximal edge of the FDS muscle1,2,6) (Fig. 18).
The ligament of Struthers is a fibrous vestige that extends from the anteromedial aspect of the distal humerus to the medial epicondyle. It is present in up to 2.7% of individuals. However, it rarely causes compression of the median nerve, accounting for only 0.5% of cases. This ligament usually originates from a supracondylar spur of the humerus, which is found in approximately 1% of the population, if such a spur exists8).
Compression of the median nerve manifests in two distinct presentations: pronator syndrome is characterized by patients experiencing pain and paresthesias similar to those seen in CTS. On the other hand, AIN syndrome primarily presents with muscle weakness. Those affected by pronator syndrome typically feel pain and paresthesia in the volar regions of the elbow, forearm, and hand. This condition affects the first to third digits, as well as the lateral half of the ring finger1,12). These hand symptoms closely resemble those observed in CTS. Both conditions may worsen with overuse. However, pronator syndrome may also include palm numbness due to compression of the palmar cutaneous nerve, which is less commonly seen in CTS. CTS often causes symptoms that disrupt sleep patterns3,12). In patients with CTS, a positive Tinel sign is typically found over the wrist. However, in patients with pronator syndrome, it is manifested over the elbow and proximal forearm3,12). Furthermore, if symptoms are reproduced when resisted forearm pronation is performed, it indicates that there may be compression of the median nerve by the pronator teres muscle. On the other hand, if symptoms are reproduced during resisted elbow flexion and supination, it suggests compression of the median nerve by the biceps aponeurosis12).
2. AIN syndromePatients with AIN syndrome, also called Kiloh-Nevin syndrome, usually experience motor weakness. One common sign of this weakness is difficulty in pinching the thumb and index finger together, often assessed by attempting to make an "OK" sign with the hand. This weakness is caused by impairment of the FPL and FDP muscles in the index finger1,3,12) Furthermore, AIN syndrome can be triggered by nonmechanical factors like Parsonage-Turner syndrome (acute brachial neuritis). This condition can cause symptoms to arise following an initial phase of shoulder pain12,14).
Compression of the AIN can occur at various points along its course1,3,12). The nerve can be trapped by either the pronator teres muscle or the proximal edge of the FDS muscle. Compression may also occur due to masses or other space-occupying lesions in the forearm. Furthermore, repetitive elbow flexion or forearm pronation can worsen the compression of the nerve.
3. CTSThe carpal tunnel is a confined fibro-osseous space, with the dorsal border formed by the volar aspects of the carpal bones and the ventral border formed by the flexor retinaculum. This retinaculum is a gently convex fibrous structure that extends from the tip of the hook of the hamate to the pisiform medially, and to the trapezium and scaphoid laterally. Within the carpal tunnel, there are nine tendons (consisting of the four FDS tendons, four FDP tendons, and the FPL tendon) as well as the median nerve, which is situated along the superficial volar aspect of the tunnel. The proximal boundary of the tunnel is marked by the scaphoid-pisiform level, while the distal end extends to the trapezium-hamate level.
Nerve entrapment can happen in the carpal tunnel when there are anatomical abnormalities that cause the canal to become smaller or the contents of the tunnel to increase. This can lead to symptoms like nighttime pain, clumsiness in the hand, tingling sensations, and numbness in the areas served by the median nerve. Usually, sensory issues come before motor problems. During a physical exam, patients with long-term conditions may show muscle wasting in the thenar eminence (Fig. 19). Additionally, they may demonstrate a positive Tinel sign and Phalen maneuver.
The diagnosis of CTS typically relies on a patient's history and clinical symptoms, along with nerve conduction studies (NCS) and electromyography. Electrophysiological assessments are also used to rule out other conditions such as polyneuropathy, plexopathy, and radiculopathy. However, they do not provide detailed spatial information about nerve anatomy and surrounding structures beyond indicating lesion levels. On the other hand, ultrasound allows for direct visualization of anatomy and nerve morphology with greater clarity. Ultrasound has comparable sensitivity and slightly superior specificity compared to NCS and electromyography in diagnosing CTS, making it a viable alternative diagnostic tool16). The traditional criteria used for diagnosing CTS with ultrasound focus on three main features: enlargement of the median nerve at the proximal carpal tunnel, palmar bowing of the flexor retinaculum, and flattening of the median nerve at the distal end (flattening ratio)10). Among these criteria, the cross-sectional area (CSA) of the median nerve at the proximal carpal tunnel is the most commonly utilized ultrasonographic measurement for diagnosing CTS (Fig. 19)16). There is a considerable range in the reported cut-off values for CSA on ultrasound, ranging from 9 to 14 mm²15).
Additionally, the CSA of the median nerve at the level of the pisiform bone, as well as the difference in CSA between the wrist and forearm, have shown to be highly effective for diagnostic purposes. The specific cut-off values for these measurements are set at 10 mm² and >2 mm², respectively7).
The differential diagnosis of CTS includes various conditions that may cause symptoms like pain, numbness, tingling, or weakness in the arm or hand. These conditions, which primarily affect the median nerve or are limited to it, consist of cervical spine disorders, brachial plexopathy, lesions in the proximal median nerve, and different types of polyneuropathy. It is crucial to differentiate CTS, especially when there is thenar muscle atrophy, from motor neuron diseases like amyotrophic lateral sclerosis (ALS) and neurogenic thoracic outlet syndrome (NTOS) that affect the lower trunk of the brachial plexus. In contrast to CTS, which only causes atrophy in the median nerve-innervated thenar muscles, ALS typically leads to selective wasting of hand muscles, including the APB and first dorsal interosseous (FDI), while hypothenar muscles like the abductor digiti minimi (ADM) are relatively preserved. This distinct pattern of muscle atrophy in the hand is referred to as the 'split hand'4). In contrast, the Gilliatt-Sumner hand, a hallmark of NTOS, is characterized by predominant atrophy of the APB muscle, additional atrophy of the FDI and ADM muscles, and preserved sensation in the median nerve-innervated region (including the thenar eminence)9).
CONCLUSIONSyndromes involving the entrapment of the median nerve exhibit specific symptoms and signs during physical examination. Ultrasonography is an effective imaging technique for identifying any structural factors that contribute to the entrapment and confirming the diagnosis. To accurately diagnose median nerve entrapment syndromes, it is crucial to have a comprehensive understanding of the nerve's anatomy, experience in assessing muscles innervated by the median nerve, and knowledge of potential compression sites along its path.
Fig. 1.Anatomical course of the median nerve. The median nerve arises from the lateral and medial cords of the brachial plexus, courses through the anterior part of the arm, forearm, and hand, and passes through the carpal tunnel. 
Fig. 2.A transverse ultrasound image obtained over the anterior aspect of the right mid-arm. The median nerve (arrowheads) runs alongside the brachial artery (arrow), positioned between the biceps brachii (above) and brachialis (below). 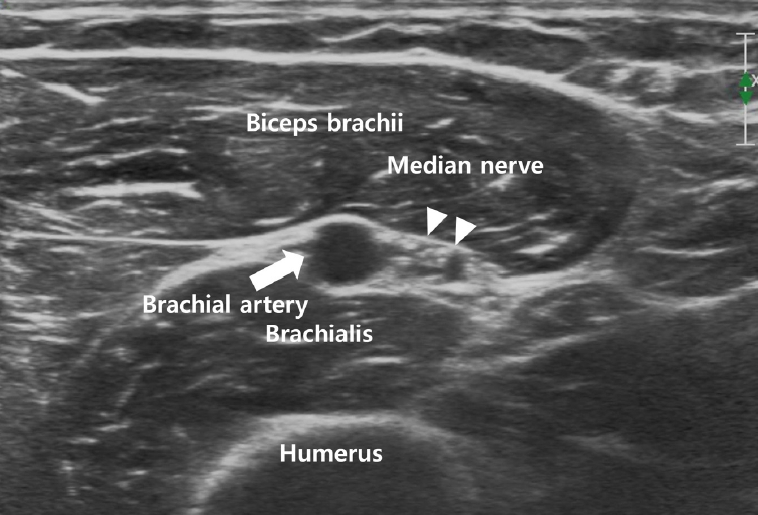
Fig. 3.A transverse ultrasound image obtained at the right proximal forearm. The median nerve (arrowheads) passes through the cleft between two heads of the pronator teres muscle, with the ulnar head (white star) positioned deep and the humeral head superficial. 
Fig. 4.A transverse ultrasound image obtained at the right mid-forearm. The median nerve (arrowheads) is positioned beneath the flexor digitorum superficialis but superficial to the underlying flexor digitorum profundus. 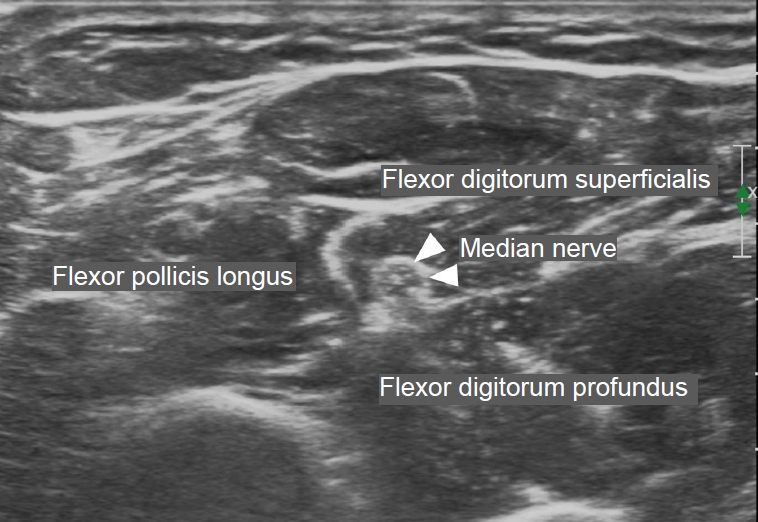
Fig. 5.A transverse ultrasound image obtained at the left wrist. The median nerve (arrow) enters the hand through the carpal tunnel, deep to the flexor retinaculum (arrow heads) along with the nine tendons of the flexor digitorum superficialis, flexor digitorum profundus, and flexor pollicis longus. 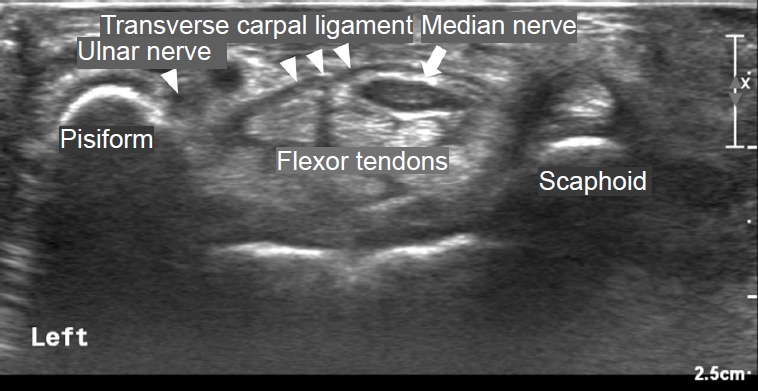
Fig. 6.Motor innervation of the median nerve. The muscles innervated by the median nerve are divided into four sequential groups (proximal forearm, anterior interosseous, thenar, and terminal). 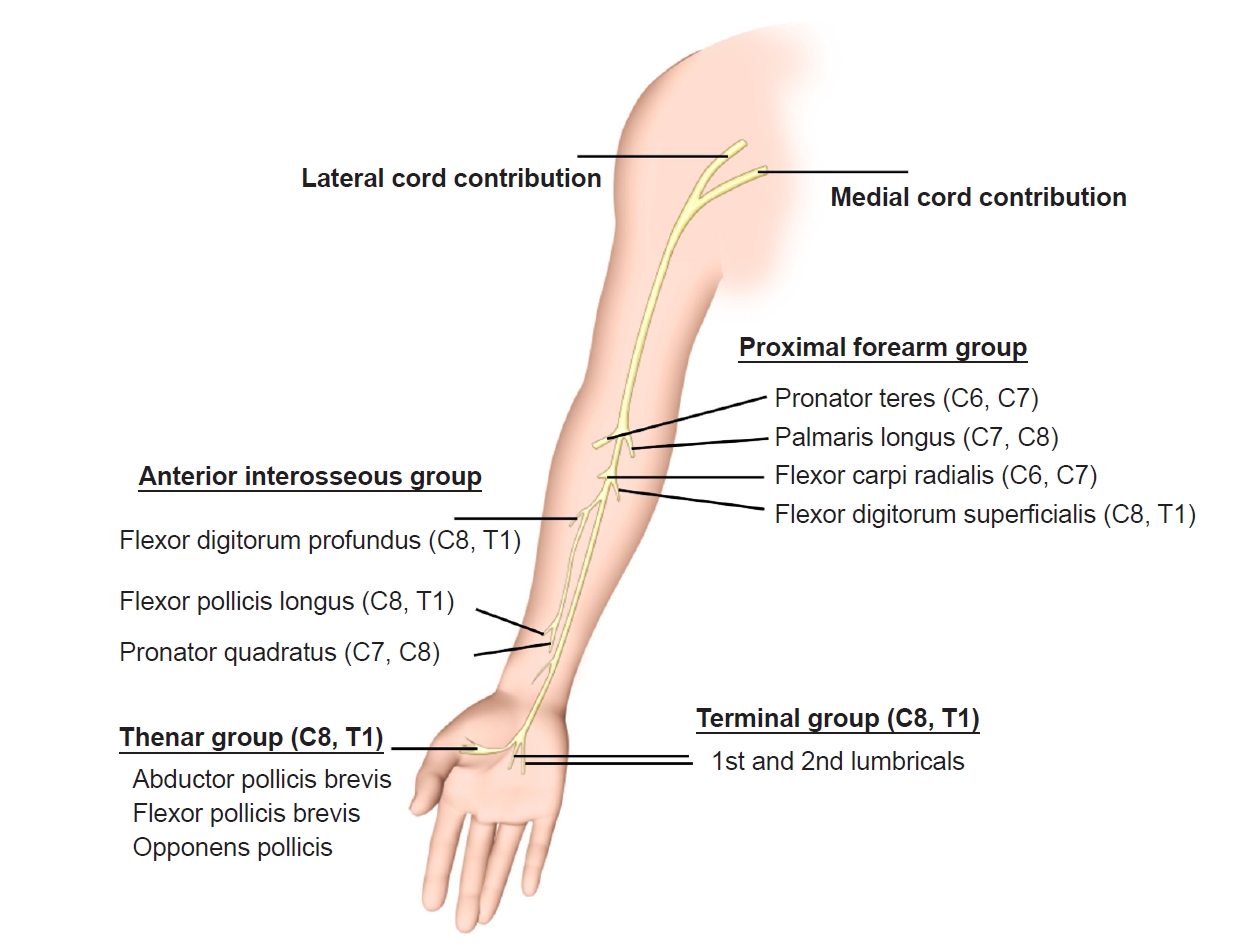
Fig. 7.Median nerve-innervated muscles in the superficial and intermediate compartment of the anterior forearm. Pronator teres, flexor carpi radialis, palmaris longus and flexor digitorum superficialis. 
Fig. 8.Flexor digitorum superficialis assessment. The patient is instructed to flex the proximal interphalangeal joint against resistance, while the other three fingers are held fully extended to deactivate the flexor digitorum profundus. 
Fig. 9.Anterior interosseous nerve-innervated muscles in the deep compartment of the anterior forearm. Flexor digitorum profundus (the lateral half acts on the middle and index fingers), flexor pollicis longus, and pronator quadratus. 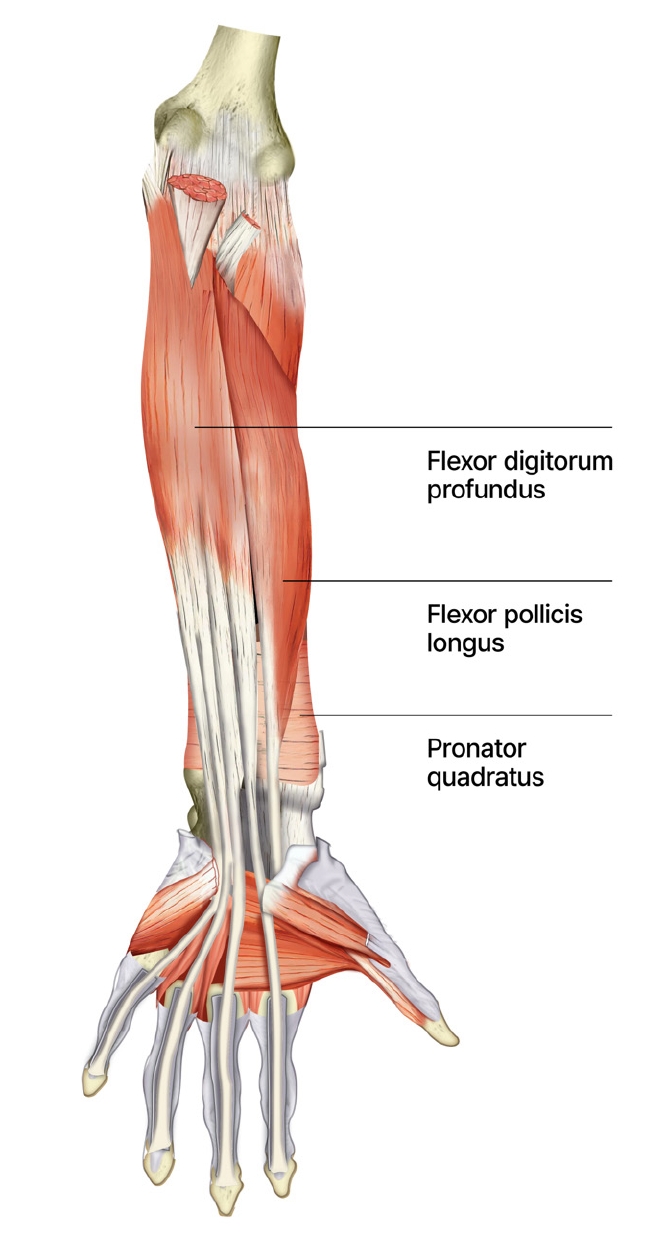
Fig. 10.Flexor digitorum profundus assessment. The patient is instructed to flex the distal interphalangeal joint of the second digit against resistance, while keeping the metacarpophalangeal and proximal interphalangeal joints immobile. 
Fig. 11.Flexor pollicis longus assessment. The patient is directed to flex the distal phalanx of the thumb against resistance, while stabilizing the thumb. 
Fig. 12.Median nerve-innervated hand intrinsic muscles. Abductor pollicis brevis, flexor pollicis brevis (superficial head), opponens pollicis and lumbricals (first and second). 
Fig. 13.Abductor pollicis brevis assessment. The patient is directed to resist thumb movement away from the palm's plane (palmar abduction), while the remaining fingers' metacarpals are immobilized. 
Fig. 14.Flexor pollicis brevis assessment. The patient is instructed to flex at the metacarpophalangeal joint, while the thumb's interphalangeal joint is immobilized. 
Fig. 15.Opponens pollicis assessment. The patient is directed to firmly press the volar pads of the distal thumb and fifth digit together, while the examiner attempts to pull the distal first metacarpal away from the fifth digit. 
Fig. 16.Lumbrical assessment. The patient is instructed to extend the index finger at the proximal interphalangeal joint, while the index finger is stabilized in the hyperextended position at the metacarpophalangeal joint. 
Fig. 17.Sensory innervation of the median nerve. The median nerve transmits cutaneous sensory signals from the radial two-thirds of the palm and the volar surfaces of the first, second, third, and radial half of the fourth digit. 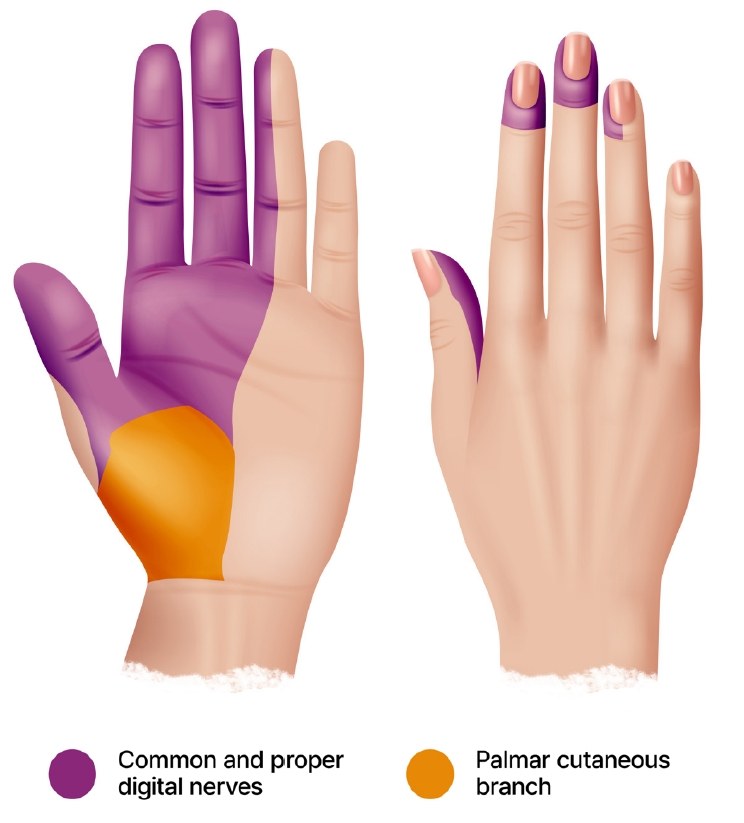
Fig. 18.Four entrapment sites around the elbow of the pronator teres syndrome. The ligament of Struthers (A), thickened biceps aponeurosis (B), between the superficial and deep heads of the pronator teres muscle (C), and thickened proximal edge of the flexor digitorum superficialis muscle (D). 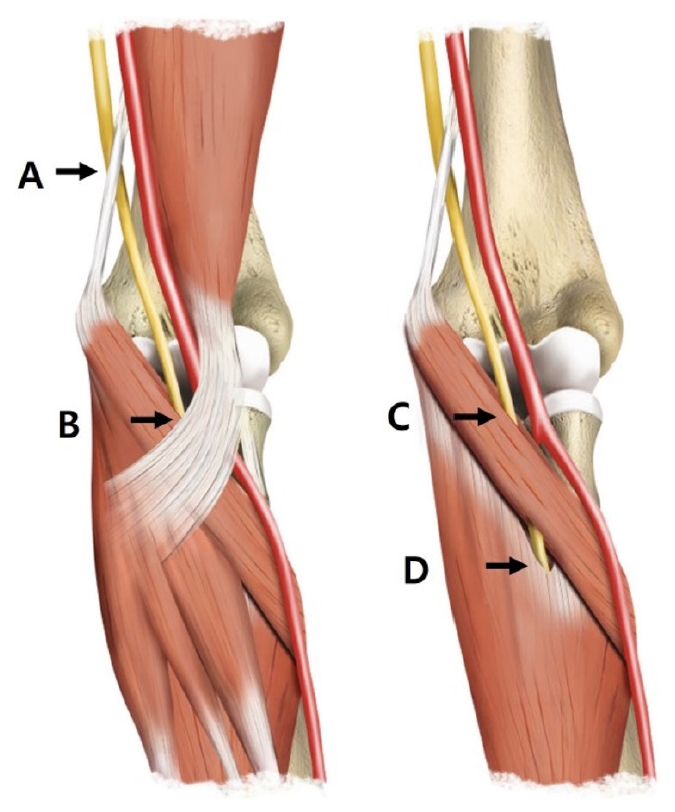
Fig. 19.Photographs of both hands in a 71-year-old patient show atrophy of the right abductor pollicis brevis muscle (ape hand deformity) (arrow) (A, B) and incomplete opposition of the thumb and little fingers (arrowhead) (C). A transverse ultrasound image at the proximal carpal tunnel demonstrates the swollen median nerve (cross-sectional area, 29.2 mm²) (arrow) (D), and a longitudinal ultrasound image reveals the median nerve flattened deep to the transverse carpal ligament (arrowheads) (E). 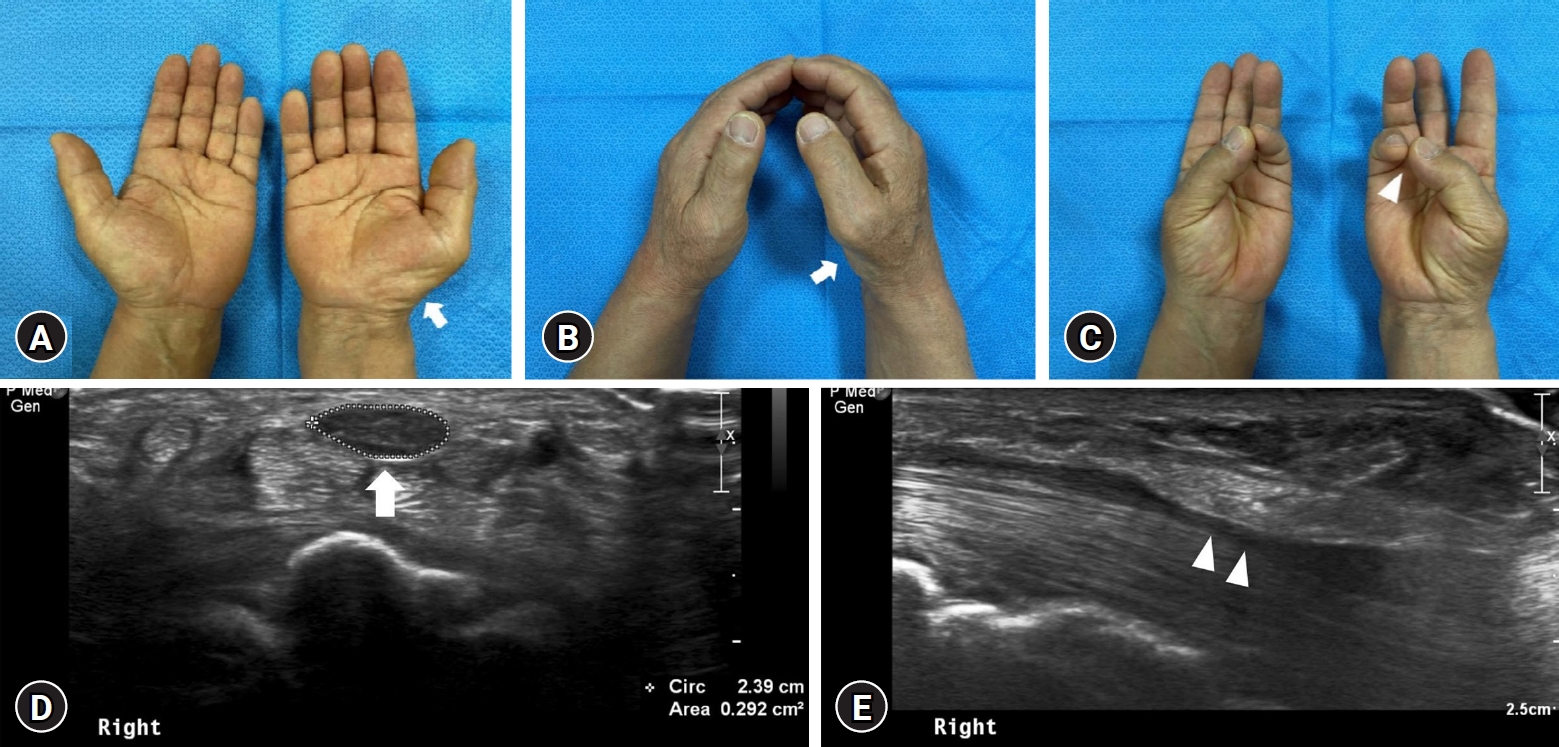
Table 1.Median nerve-innervated muscles and actions REFERENCES1. Andreisek G, Crook DW, Burg D, Marincek B, Weishaupt D: Peripheral neuropathies of the median, radial, and ulnar nerves: MR imaging features. Radiographics 26:1267-1287, 2006
2. Bilecenoglu B, Uz A, Karalezli N: Possible anatomic structures causing entrapment neuropathies of the median nerve: An anatomic study. Acta Orthop Belg 71:169-176, 2005
3. Dang AC, Rodner CM: Unusual compression neuropathies of the forearm, part II: Median nerve. J Hand Surg Am 34:1915-1920, 2009
4. Eisen A, Kuwabara S: The split hand syndrome in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 83:399-403, 2012
5. Garg K: BD Chaurasia’s human anatomy: Regional and applied, dissection and clinical, ed 5th. New Delhi, IN: CBS Publishers & Distributors, 2010
6. Lee MJ, LaStayo PC: Pronator syndrome and other nerve compressions that mimic carpal tunnel syndrome. J Orthop Sports Phys Ther 34:601-609, 2004
7. Linehan C, Childs J, Quinton AE, Aziz A: Ultrasound parameters to identify and diagnose carpal tunnel syndrome. A review of the literature. Australas J Ultrasound Med 23:194-206, 2020
8. Lordan J, Rauh P, Spinner RJ: The clinical anatomy of the supracondylar spur and the ligament of Struthers. Clin Anat 18:548-551, 2005
9. Matsubara T, Kurokawa K, Sakurai K, Yasutomi H, Yamawaki T: The Gilliatt-Sumner hand: A diagnostic clue of neurogenic thoracic outlet syndrome. QJM 111:831-832, 2018
10. Miller TT, Reinus WR: Nerve entrapment syndromes of the elbow, forearm, and wrist. AJR Am J Roentgenol 195:585-594, 2010
11. Russell SM: Examination of peripheral nerve injuries: An anatomical approach, ed 2nd. New York, NY: Thieme, 2015
12. Tsai P, Steinberg DR: Median and radial nerve compression about the elbow. Instr Course Lect 57:177-185, 2008
13. Wikipedia. Median nerve. San Francisco, CA: Wikimedia Foundation, Inc, 2024 (https://en.wikipedia.org/wiki/Median_nerve) [Accessed Feb 23, 2024]
14. Wong L, Dellon AL: Brachial neuritis presenting as anterior interosseous nerve compression-implications for diagnosis and treatment: a case report. J Hand Surg Am 22:536-539, 1997
|
|
|||||||||||||||||||||||||||||||||||||