Suitability of Cervical Oblique Magnetic Resonance Imaging for Surgical Planning
Article information
Abstract
Objective
Objective: Our aim was to calculate the diagnostic power, including positive predictive value (PPV), of cervical oblique magnetic resonance imaging (MRI), and to identify cases in which its use led to altered surgical plans.
Methods
Two hundred eighty-nine patients, who underwent 1- or 2-level anterior cervical discectomy and fusion from January 2015 to December 2017, were included in this study. Medical records were reviewed. Statistical analysis was performed to assess the equality of the 2 groups, with or without cervical oblique MRI. We attempted to determine the diagnostic power of cervical oblique MRI by evaluating PPV in specific cases.
Results
The 2 groups were not significantly different in age, sex, operation time, preoperative visual analog scale (VAS), postoperative VAS. If we set diff-VAS (preoperative minus postoperative VAS) as ≥1, PPV of cervical oblique MRI was 86.76%, whereas PPV of conventional MRI was 72.35%. Each calculated PPV was higher with cervical oblique MRI. Furthermore, we identified 11 patients (8.09%) who experienced a change in surgical plan because of cervical oblique MRI. Measured widths of the foramen were 3.69 mm in axial images and 3.31 mm in oblique images.
Conclusion
Cervical oblique MRI can enable a more accurate surgical plan and facilitate patient selection for surgery. Cervical oblique MRI could be useful for additional information and to predict the immediate prognosis of patients preoperatively.
INTRODUCTION
Cervical foraminal stenosis induces cervical radiculopathy and is often caused by a herniated disc or osteophytes. The progressive narrowing of the cervical foramen could result in nerve entrapment and inflammation, leading to irreversible dysfunction of the nerve3).
Magnetic resonance imaging (MRI) is commonly used for the diagnosis and evaluation of herniated cervical discs (HCDs). MRI can discriminate soft tissue from bone and spinal cord; however, conventional MRI is limited in that it shows only sagittal and axial images of the cervical spine2). Since the cervical foramen of the spine is very subtle to reveal, cervical oblique MR images have recently been used to highlight cervical foraminal stenosis10). Regarding lumbar stenosis, there has been a study revealing the diagnostic value of oblique lumbar MRI. In this study, oblique lumbar MRI was useful in diagnosing extraforaminal lumbar disc herniation and was found to affect the surgical plan4).
Several studies have provided a grading system for cervical oblique MRI and its clinical correlation5–8,11). Many of those studies involved foraminal size and visible nerve root compression as detected by cervical oblique MRI; notably, we could not find reports regarding the relationship between cervical oblique MRI and a clear impact on surgical planning. Further, although every diagnostic tool possesses specific diagnostic characteristics (e.g., a certain level of sensitivity or specificity), there has been no attempt to investigate these in cervical oblique MRI. Therefore, we herein attempt to establish the diagnostic power of cervical oblique MRI and to simultaneously determine whether it influences surgical planning.
MATERIALS AND METHODS
1. Patients
This was a retrospective cohort study that spanned from January 2015 to December 2017. A total of 7,325 patients visited the outpatient clinic of our institution (Gangnam Severance Hospital, Yonsei University College of Medicine); we excluded patients with tumor, trauma, myelopathy patients, ossification of the posterior longitudinal ligament, multiple HCDs including more than 2 discs, recurrent disc, and those who underwent a posterior approach or previous surgery to correct a cervical disc (Fig. 1).

Schematic flowchart of the study. The 289 patients were enrolled in this study and divided into two groups according to the presence of the cervical oblique magnetic resonance imaging (MRI). Only degenerative cervical radiculopathy patients were included in this study. ACDF: anterior cervical discectomy and fusion; OPLL: ossification of the posterior longitudinal ligament; ASD: adjacent segment disease.
Finally, 173 males and 116 females were included in this study, total 289 patients; these patients were divided into two groups based on the presence of cervical oblique MRI (without cervical oblique MRI, 153; with cervical oblique MRI, 136).
The mean age of the population was 50.6 years (range, 19–79 years). Every patient was evaluated for preoperative and post-operative pain score[assessed by visual analog scale (VAS)] and operation time. Postoperative pain score was obtained just after recovery after anesthesia. Based on postoperative pain relief, we attempted to compare the positive predictive value (PPV) between the 2 groups. Additionally, ethical approval was obtained from the Institutional Review Board (IRB) of our institution (IRB no. 2017-0953-002, 3-2018-0015), as specified in the Declaration of Helsinki.
2. MRI Imaging and Measurement
In the outpatient clinic, every patient suspicious for degenerative cervical disc was evaluated by conventional MRI. If the finding of the MRI seems to be not symptomatic, physicians ordered to precede the cervical oblique MRI to investigate foramen more precisely.
We attempted to determine how many patients underwent a change in treatment plan based on the results of their cervical oblique MRI. First, the surgical plan was established, based on sagittal and axial MR images, then it was compared with oblique MRI. During this procedure, we identified patients who underwent a change in treatment modality; these were further investigated in terms of the foraminal width, as well as the axial and oblique foraminal grade of the lesion. Foraminal width was measured as the longest width of the foramen from axial and oblique images.
3. Calculation of PPV
The PPV is defined as the number of true positives divided by the number of positive calls. We presumed that immediate postoperative pain relief could be an indication of the presence of HCD. Thus, in this study, the number of positive calls was defined as the number of patients who showed positive findings in MRI. The number of true positives was defined as the number of patients who experienced immediate postoperative pain relief. The immediate postoperative pain relief was then calculated as diff-VAS; preoperative VAS minus postoperative VAS. We stratified the number of true positives by the diff-VAS.
The characteristics of the 2 groups were analyzed by independent 2-samples t-test and chi-squared test. PPVs were calculated by the number of patients who experienced pain relief divided by the total number of patients in each group. All statistical analyses were performed using SPSS version 21.0 (SPSS Inc., Chicago, IL, USA), with a p-value <0.05 considered statistically significant.
RESULTS
1. Patient Population
The statistical power of each variable is shown in Table 1. There were no statistically significant differences in the sex, age, operation time, level, postoperative VAS, except preoperative VAS (p=0.023).
2. PPV
We divided the results into two different situations: cases with and without myelopathy. PPV was analyzed according to immediate pain relief (diff-VAS; preoperative VAS minus post- operative VAS), such that diff-VAS=1, 2, or 3 for each situation. The PPVs of cervical oblique MRI were determined as 86.76% (diff-VAS 1), 74.26% (diff-VAS 2), and 61.02% (diff-VAS 3). Conversely, the PPVs of conventional cervical MRI were determined as 82.35% (diff-VAS 1), 70.58% (diff-VAS 2), and 54.24% (diff-VAS 3) (Table 2).
3. Change in Treatment Modality Based on Cervical Oblique MRI
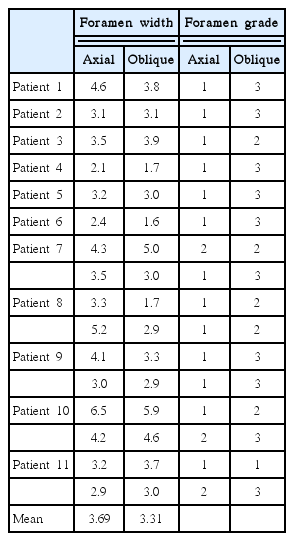
A total of 153 Patients without cervical oblique MRI were excluded from this portion of the analysis. Among 136 patients with cervical oblique MRI, 11 patients (8.09%) were identified who underwent a change in treatment plan from conservative care to invasive surgery. We measured each width, as well as the axial and oblique grade of each cervical foramen that underwent an operation. Mean values of the foramen width were 3.69 mm in axial images, with a range of 2.1 to 6.5 mm, and 3.31 mm in oblique images, with range of 1.6 to 5.9 mm without statistical significance (Table 3).
DISCUSSION
HCD causes several symptoms by compressing either the spinal cord in the central spinal canal or the nerve root in the spinal foramen. This process may cause pain, tingling, numbness, and further weakness of the muscle. Though HCD is diagnosed by physical exam, plain radiography, and/or other exams, most surgeons depend on MRI methodology to discriminate the specific compressive lesion and guide the surgical planning process7). Oblique MRI might have the potential to alter surgical plans and increase diagnostic accuracy6). Park et al.7) reported that diagnosis with an oblique view can be improved by 1.0%, from 91.3% with conventional MRI. However, this number might be misunderstood, as the study focused on the detection of the exact disc level in patients with perfect pain-relief.
The purpose of the current study was to determine the comparative PPV of cervical oblique MRI, which can thus help clinicians to predict prognosis after surgery, with a prospective view of pain. Adogwa et al.1) demonstrated that immediate post- operative pain score accurately predicts and correlates with 1-year pain score after an anterior cervical discectomy and fusion (ACDF) procedure. Thus, we hypothesized that patients who experienced immediate pain relief were diagnosed and treated appropriately based on MRI findings. Moreover, we focused on the impact of cervical oblique MRI on the surgical plan. In our institute, we did not routinely conduct cervical oblique MRI; rather, under special conditions, we requested cervical oblique MRI. We attempted to identify the PPV of cervical oblique MRI by defining “disease” as pain relief in accordance with the hypothesis that every patient may exhibit positive findings in MRI. There were no statistical differences between the conventional MRI group and the cervical oblique MRI group. At all set points of pain relief, we found superiority of cervical oblique MRI by 3.11% to 6.12% in terms of PPV. The statistics were indicative of better PPV in patients with myelopathy than in those without myelopathy; this result may be confusing, as cervical oblique MRI is mainly focused on neural foraminal stenosis. However, as early surgery is easily confirmed in myelopathy patients, it may be that more immediate pain relief is observed in these patients because of the lesser degree of cumulative nerve damage. The PPVs of conventional MRI and cervical oblique MRI were measured as approximately 80%, in contrast with the report by Park et al.9). However, the extent of difference between conventional and cervical oblique MRI was similar between our study and the previous study.
Further, we attempted to identify surgical cases that under-went a change from conservative care to discectomy; notably, we found 16 discs of 11 patients among 136 patients. These patients showed grade 1 foraminal stenosis without central stenosis and were designated to be observed in the outpatient clinic. In cervical oblique MRI, most patients were identified as grade ≥2 and were then scheduled to undergo surgery with the detection of grade 1 stenosis in axial images. The measured width of the foramen differed between axial and oblique MRI. However, because of a lack of numbers, we could not calculate the statistical difference. A typical case involving a change in surgical plan is shown in Fig. 2, where we were convinced by cervical oblique MRI. In the Fig. 2, there was severe foraminal stenosis on right side of C5/6 but we were not so sure whether the lesion of C6/7 could be symptomatic. While sagittal and axial images do not reach surgical indication, it was obvious in the oblique images. According to these findings, we decided to operate not only C5/6 but C6/7. She experienced immediate pain relief on right shoulder showing diff-VAS 4. These findings imply that about 8% of patients could have surgical lesion that was not found on conventional MRI.

Typical usefulness of oblique magnetic resonance imaging. (A) Sagittal image of the pathologic lesion (C5–6 and C6–7), it is easily observed on C5–6 stenosis, but it seems to be not enough to operate C6–7. (B) Axial image of the C5–6. Mild stenosis on right side foramen is observed. (C) Axial image of the C6–7. Also, mild stenosis on right side foramen is observed. (D) Oblique image of the pathologic lesion, it is clearly shown that foraminal stenosis of C5–6 and C6–7, helping to decide the surgical plan.
This study has several limitations. First, factors that could influence postoperative pain relief were not included, such as smoking, alcohol, duration of symptoms, osteoporosis, or bone morphogenetic protein use. Second, this study contains patients who underwent 1- or 2-level ACDF. There may be confounding factors in two-level ACDF patients, which distinguish them from one-level ACDF patients. However, because of the need for statistical power, we included two-level ACDF patients in this analysis; notably, this might lead to a misunderstanding regarding PPV. Thus, this study should be best viewed in terms of guidelines, rather than absolute measures. Third, as only inpatients were involved in this study, outpatient data was not included. Thus, this study involves cases that whose plans were changed from observation to surgery, but not from surgery to observation; these downgraded cases are critical to identify the sensitivity of the cervical oblique MRI. Fourth, not every patient had cervical oblique MR images in this study, as a result of the patient characteristics that were described above. Fifth, immediate pain relief does not discriminate neck and arm VAS; critically, there was no data regarding neck disability index or Oswestry disability index.
Despite the limitations, cervical oblique MRI could predict immediate postoperative pain relief and even contribute to a change in surgical plan. Because cervical oblique MRI does not incur an additional expense and may be helpful for surgery, some surgeons have begun to routinely request cervical oblique MRI assessments of their patients. Notably, we could not determine specificity, which could shift a surgical plan to observation by excluding false lesions. Further studies might be needed to clearly characterize the diagnostic value of the cervical oblique MRI.
CONCLUSION
This study provides an assessment of the PPV of cervical oblique MRI in HCD patients, in a manner that could be performed in the clinic. We observed immediate postoperative pain relief in approximately 80% of patients who have positive findings in oblique MRI. Moreover, with use of cervical oblique MRI, we were able to obtain a more accurate diagnosis for surgery than with use of conventional MRI.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.