The Efficacy of Percutaneous Cervical Nucleoplasty for Cervical Herniated Disc Disease in Patients with Upper Extremities Radiating Pain
Article information
Abstract
Objective
Percutaneous cervical nucleoplasty is a minimally invasive intervention used to perform disc decompression in cases of pain caused by disc herniation. Here, we describe the efficacy of nucleoplasty for the treatment of cervical disc herniation in patients with upper extremities radiating pain.
Methods
From March 2015 to March 2016, we performed percutaneous cervical nucleoplasty in 32 consecutive patients and evaluated short-term follow-up results (until three months) after the procedure. Patients were evaluated via neurological examination, and using the visual analogue scale (VAS) before and after the procedure. Patients with motor weakness, myelopathy, and spinal instability were excluded.
Results
The age of patient sample ranged from 30 to 80 years old (mean 52.63), with males outnumbering females by 17 to 15. The procedures were performed at a single level in 30 cases and two levels in two cases. The C5-6 level was the most commonly affected. The mean VAS scores of pre- and postprocedure were 6.91±0.54 and 2.69±0.35, with a statistically significant decrease in the mean VAS score by 4.22±0.91 (p<0.001). The mean VAS score increased from day one to three months postprocedure (p=0.02) but was still significantly lower than the preprocedure mean VAS score. In extrusion cases, the differences in the VAS scores at preprocedure, day one and three months postprocedure were statistically significant (p<0.001).
Conclusion
Percutaneous cervical nucleoplasty can be used as a minimally invasive treatment in patient with cervical herniated disc accompanied with radiating pain, as it is a safe and efficacious procedure.
INTRODUCTION
Cervical herniated intervertebral disc can cause various symptoms including posterior neck pain, shoulder or arm radicular pain, and numbness. In cases where conventional treatments such as pharmacological intervention, physical therapy, and nerve root block are ineffective, anterior cervical discectomy and fusion (ACDF) surgical treatment can be considered along with standard treatment2,11,12,15,16). It is very effective in terms of symptom remission, but risks involved include complications related to general anesthesia, limited neck motion, visible scars, and airway compression. Various minimally invasive treatments were recently developed, and the safety and effectiveness of percutaneous cervical nucleoplasty in particular has been proven in numerous studies1,2,5–7,9–16). The purpose of this study was to assess the efficacy of percutaneous cervical nucleoplasty and short-term prognosis in patients with ruptured cervical disc presenting radicular pain in the upper extremities.
MATERIALS AND METHODS
1. Patients
This study was conducted on 32 patients with ruptured cervical disc treated with cervical nucleoplasty between March 2015 and March 2016 at our hospital. The study was approved by the hospital’s medical research ethics committee, and written informed consent was obtained from all patients before the nucleoplasty procedure. The study was performed in accordance with the principles embodied in the Declaration of Helsinki.
Patients presented to our hospital with posterior neck pain with shoulder or arm radiating pain. Physical examination, X-ray, and magnetic resonance imaging (MRI) were conducted to diagnose herniated disc in the cervical spine. Nucleoplasty was conducted when presenting symptoms were in accordance with the examinations performed in patients with no symptom improvement despite conventional pain management using medication, physical therapy, and root blocks. Patients with protruded or extruded cervical discs were included and with motor weakness, myelopathy, and spinal instability were excluded. The morphology of intervertebral disc was defined as protrusion and extrusion by the intactness of annulus.
2. Procedure
Nucleoplasty was conducted under sterile conditions by three neurosurgeons using INTO-CB by Intocare corp. (Yangju, Korea). The patient was placed in the supine position on the table, a gel pad was placed under the neck so that it was slightly hyperextended to facilitate access to the cervical disc. The C-arm was positioned to obtain an anteroposterior (AP) view to confirm the target disc level. After the internal carotid artery was laterally displaced with the surgeon’s index and middle fingers, the needle entry site was secured. Then, the needle was introduced via the paratracheal approach till it reached the anterolateral annulus fibrosus. Lidocaine (2%) was administered from the disc to the skin while checking that blood was not aspirated by means of repeated suction and injection. Under the C-arm fluoroscope guidance, a 19-gauge introducer needle was introduced at the entry point at about a 40° angle using the paratracheal approach until it reached the annulus fibrosus. After the lateral and AP view were obtained confirming the location of the needle-tip, the lateral view was used to advance the introducer needle into the intervertebral disc. The stylet of the introducer needle was withdrawn, and the INTO-CB (spinal wand) was replaced and advanced further. Coagulation was tested with 1 to 2 sec radiofrequency to confirm that there was no movement or paresthesia in the patient’s upper limbs. Guided by the C-arm fluoroscope, coblation was then carried out by 180° rotation of the flange. Ablation was done for 20 to 60 sec and retreated several times to coagulate the intervertebral disc. The procedure took an average of 15 min, and no specific discomfort was noted in patients during the procedure. After the procedure, patients were placed on complete bed-rest in the supine position for four hr. Patients were discharged a day after the procedure and visited the outpatient clinic 3 months after the procedure to evaluate the efficacy of the procedure using the visual analogue scale (VAS) (Fig. 1).
The patient was a 45-year-old female who had been suffering from right shoulder radiating pain for a year. Cervical magnetic resonance imaging showed the disc protrusion with mild cord indentation at C5-6 intervertebral disc level; sagittal (A) and axial (B) image. Nucleoplasty was conducted using INTO-CB with C-arm fluoroscope guidance. After the internal carotid artery was laterally displaced with surgeon’s index and middle fingers (C), coblation was carried out in lateral view to confirm the place of tip (D).
3. Statistical Analyses
The statistical analyses were performed using SPSS version 22 for Windows (SPSS Inc., Chicago, IL, USA). The individual data were expressed as mean±standard deviation (SD). A paired t-test was used to compare the results of nucleoplasty at preprocedure day one and three months postprocedure. The level of statistical significance was set at p<0.05.
RESULTS
Of the 32 patients, 17 were male and 15 female, indicating a greater proportion of male patients. The age of patients ranged from 30 to 80 years with a mean age of 52.63 years. There were three patients in their 30s, 12 cases in their 40s, 10 in their 50s, four in their 60s, two in their 70s, and one in their 80s with the maximum number of patients in the group in their 40s.
There were 30 cases of nucleoplasty at a single level and two cases at multiple levels. The procedure was classified by the disc location, with the maximum number of cases at the C5-6 level (C3-4 one case, C4-5 two cases, C5-6 17 cases, and C6-7 14 cases).
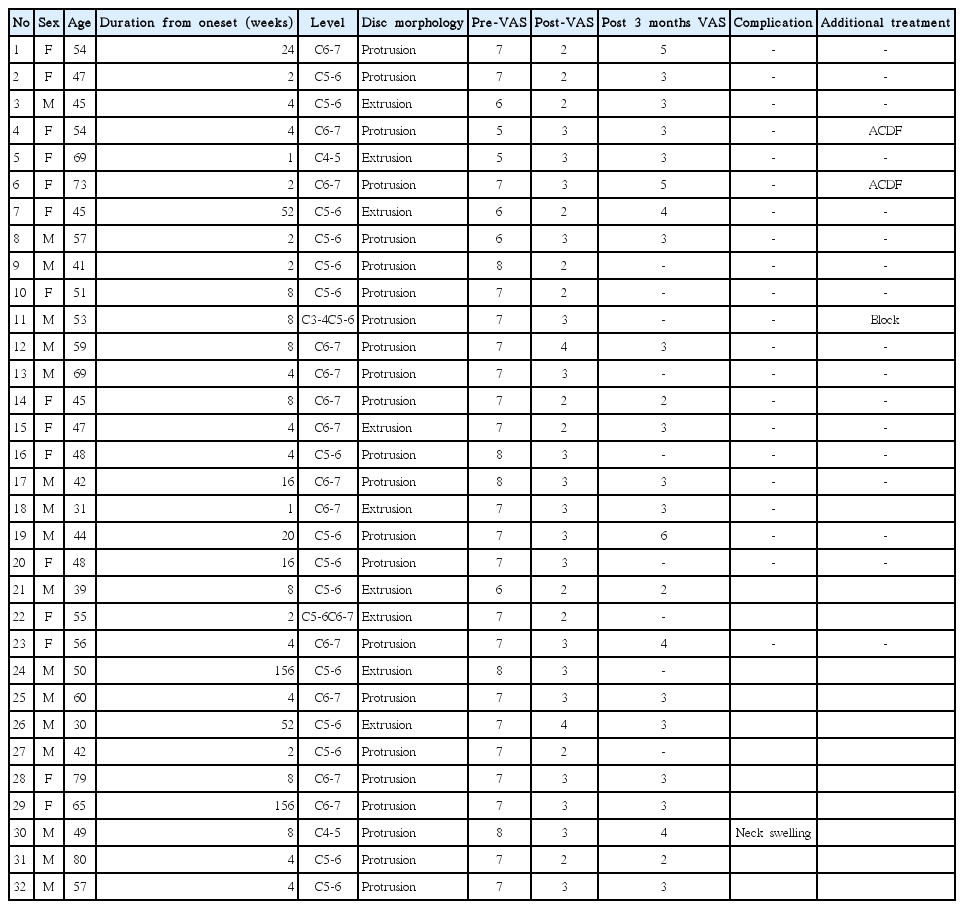
All patients reported radicular pain in upper extremities, and the patients had the symptoms for an average 18.69± 38.10 weeks. Depending on the disc morphology, disc protrusion was demonstrated in 23 cases and extrusion in nine cases (Table 1).
All 32 cases were assessed at day one postprocedure, but nine cases were lost to follow-up at three months postprocedure. Physical and neurological examination, and VAS score analysis were performed at preprocedure and one day and three months postprocedure to evaluate the intensity of pain and, neurological and residual symptoms.
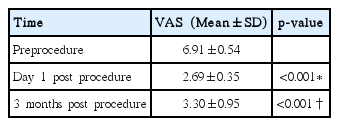
The preprocedure mean VAS score was 6.91±0.54 that improved to 2.69±0.35 with an average reduction of 4.22±0.91 at day one postprocedure. The mean VAS score at three months postprocedure improved to 3.30±0.95 with an average reduction of 3.43±1.12. The differences in the VAS scores at preprocedure, day one and three months postprocedure were statistically significant (p<0.001) (Table 2).
In the extrusion cases, the preprocedure mean VAS score was 6.63±0.84 that improved to 2.63±0.55 with an average reduction of 4.00±1.00 at day one postprocedure. At three months postprocedure, the mean VAS score improved to 3.00 ±0.40 with an average reduction of 3.29±0.95. The VAS scores at preprocedure, day one and three months postprocedure were significantly different (p<0.001) (Table 3).
There was one case with neck swelling due to a postprocedural hematoma caused by procedural complications. It did not result in a severe complication, and the patient completely recovered without any treatment. There were three cases that required additional treatment during the follow-up period - a root block was conducted in one case and ACDF were conducted in two cases of these three cases.
DISCUSSION
Percutaneous cervical nucleoplasty procedure is used for disc decompression by radiofrequency energy. Theoretically, the deneutralized proteoglycan of the target disc nucleus pulposus transforms to the liquid or gaseous state and is removed by being absorption2,12).
The coblation technique is divided into two different steps-tissue ablation and coagulation. A plasma field is generated between the spinal wand and the tissue in the ablation step that breaks the molecular bonds of the disc nucleus to generate the constituent molecules and gases. The next step involves collagen shrinkage by thermal coagulation via a moving wand. The intradiscal pressure is decreased by removing about 1 g of tissue via these two steps12,13,16). Chen et al.4) demonstrated that the coblation techniques reduce the disc pressure in a cadaveric specimen.
Percutaneous cervical nucleoplasty has been proven to be effective in the treatment of cervical disc herniation in several studies1,2,5–7,9–16). In support of this, we report that the preprocedure mean VAS score of 6.91±0.54 that improved to 2.69±0.35 at day one postprocedure and 3.30±0.95 at three months postprocedure (p<0.001). However, the VAS score, excluding nine cases that were lost to follow-up, increased from 2.74±0.38 to 3.30±0.95 from day one to three months postprocedure (p=0.02) (Table 4).

Comparison of the visual analogue scale excluding nine follow-up loss cases; Day one and three months post nucleoplasty
The nine patients were lost to follow-up after three months postprocedure, and they were considered to be recovered and did not revisit as outpatients. This might be due to reduced hospital accessibility as most of patients are working in the agriculture industry by its regional characteristics. Hence, exclusion of the nine patients who were expected have low VAS scores were influenced on increase of the VAS score at three months postprocedure. Therefore, exclusion of nine patients with expected low VAS score can affect increase in VAS core at three months postprocedure.
ACDF was conducted in two cases and root block in one case. Percutaneous cervical nucleoplasty was found to be effective in reducing pain up to three months postprocedure, but the effectiveness was lower than that at day one postprocedure.
There was one case with neck swelling as a result of complication related to the procedure which occurred by hematoma at postprocedure. The patient did not complain of dyspnea and completely recovered without any further treatment. Kim et al.8) recently presented a surgery case for hematoma due to inferior thyroid artery injury after percutaneous cervical nucleoplasty. No severe complications related to percutaneous cervical nucleoplasty were found in most of other studies thus proving that it can be considered as a safe procedure1–3,5–7,9–13,15,16).
Percutaneous cervical nucleoplasty has benefits in minimizing tissue damage and reducing the risk of complication related to general anesthesia3,7). It is also cost-effective as it shortens hospitalization period with early recovery. Hence, it can be used as a minimally invasive treatment prior to ACDF in herniated cervical disc patients with radiating pain in upper extremities.
There are some limitations in our study. Firstly, inaccuracy of data from retrospective study raises the possibility of error. Secondly, it is difficult to make a conclusion with an inadequate number of cases (32 cases). Lastly, the postprocedure observation period was limited to three months, which is not long enough to evaluate the disease prognosis. Thus, a larger number of patients with longer observation period would be necessary for further evaluation in the future.
CONCLUSION
Percutaneous cervical nucleoplasty is effective in reducing radiating pain in upper extremities of patients with herniated cervical disc that did not respond to conventional treatment. Although the effect of pain reduction decreased at three months postprocedure compared to day one postprocedure, it was still statistically significant compared to preprocedure. In addition, statistically significant pain reduction was observed in disc extrusion cases.
Percutaneous cervical nucleoplasty is a relatively safe procedure without risk of severe complications. Hence, it can be considered as a treatment modality for cervical disc herniation.