Brachial Plexus Injury in Adults
Article information
Abstract
Brachial plexus injury (BPI) is a severe peripheral nerve injury affecting upper extremities, causing functional damage and physical disability. The most common cause of adult BPI is a traffic accident, and the incidence has steadily increased since the 1980s. BPIs can be divided into three types; preganglionic lesion, postganglionic lesion, and a combination of both. Whether the continuation of the root and the spinal cord is preserved is a critical factor in determining the treatment strategy. The level of lesion can be analogized by clinical manifestations. But imaging studies including computed tomography (CT) myelography and magnetic resonance imaging (MRI) as well as electrodiagnostic studies are helpful in diagnosis of BPI. If diagnostic electromyography suggests that the damage is non-degenerative, conservative management is indicated. However, a reconstructive plan should be formulated, when there is no evidence of spontaneous recovery within 6 months of injury. Operative options used in BPI include nerve grafting, neurotization (nerve transfer), and other brachial plexus reconstructive techniques including the transplantation of various structures. In this review article, the mechanism and classification of injury, clinical manifestations, updated diagnostic studies, recent treatment strategies, and pain after BPI would be discussed.
INTRODUCTION
Brachial plexus injury (BPI) is a severe peripheral nerve injury affecting upper extremities, causing functional damage and physical disability55). The most common cause of adult BPI is a traffic accident, such as motorcycle accidents. Most patients are young men between 15 and 25 years of age2,21,29). Other traumatic causes include sports injuries, incised wounds, gunshot wounds, carrying a heavy backpack, and inappropriate operative positioning52,55). Non-traumatic causes consist of tumors, irradiation, and congenital abnormalities such as cervical ribs81). In recent literature, the prevalence rate is about 1.2% after multiple traumatic injuries, and the annual incidence is about 1.64 cases out of 100,000 people69). In this review article, the mechanism and classification of injury, clinical manifestations, updated diagnostic studies, and recent treatment strategies would be discussed.
1. Anatomy of the Brachial Plexus
The brachial plexus runs within the interscalene triangle bounded by the anterior scalene muscle anteriorly, the middle scalene muscle posteriorly and the superior border of the first rib inferiorly65). It traverses the posterior triangle of the neck, formed by the clavicle inferiorly, the trapezius muscle laterally and the posterior border of sternocleidomastoid muscle medially68). Then it passes laterally over the first rib and enters the axilla to supply the upper limb.
The brachial plexus is composed by 5 anatomical components: 5 roots, 3 trunks, 6 divisions, 3 cords, and 5 terminal branches (Fig. 1). Five roots include the anterior branches of the 4 lowest cervical spinal nerve roots (C5–C8) and the first thoracic nerve root (T1). Rarely, it is co-contributed by C4 and T2, with little clinical significance20,32,57,76). Two pairs of nerve roots extend from each segment of the spinal cord; ventral (anterior) and dorsal (posterior) roots. The ventral roots contain motor fibers exiting the spinal cord. The dorsal roots convey sensory fibers that came from the dorsal root ganglion and enter the spinal cord. The ventral and dorsal roots get together beyond the ganglion, and become the spinal nerve. These dorsal and ventral roots consist of rootlets, which are defined on magnetic resonance imaging (MRI) as 3 or 4 bands of rootlets in the upper roots (C5–C7) and 2 bands in the lower roots (C8, T1)22). At the point that the ventral and dorsal roots leave the spinal cord, the arachnoid and dura are extended and form the root sleeve. The root sleeve adheres to the ventral root and spinal ganglion, and forms the nerve sheath. For this reason, there is no extending of the cerebrospinal fluid (CSF) space beyond the intervertebral foramen. Only the nerve roots up to the level of the intervertebral foramen are visualized in myelography. Myelography cannot show the spinal nerves distal to the intervertebral foramen.
The spinal nerves join and form 3 trunks; upper, middle and lower. The upper 2 roots (C5, C6) merge into the upper trunk at Erb’s point. The middle C7 root is continued as the middle trunk. The lower 2 roots (C8, T1) join and form the lower trunk. These trunks divide into anterior-posterior (AP) divisions just above the clavicle. The lateral cord is made by the anterior divisions of the upper and middle trunks, and the medial cord is formed by the continuation of the anterior division of the lower trunk. The posterior divisions of each trunk join and form the posterior cord. The posterior cord locates posterior to the subclavian artery. The anatomical term of these 3 cords designates their association to the second part of the axillary artery.
The lateral cord is divided into two terminal branches; the musculocutaneous nerve and the lateral root of the median nerve which is called the sensory contribution. The medial cord is divided into the ulnar nerve and the medial root of the median nerve, namely ‘motor contribution’. The posterior cord is divided into the radial nerve and the axillary nerve38).
2. Pathophysiology of the BPI
Root injury is defined as root avulsion from the spinal cord and rupture in the preganglionic root zone or dorsal ganglion at the vertebral foramen. Injuries distal to the ganglion are classified as post-ganglionic injury, which divided into supra- and infraclavicular injury. Post-ganglionic supraclavicular injury includes injury of the spinal nerves, trunks and the divisions. Post-ganglionic infraclavicular injury means injury of the cords and the terminal branches.
The great range of motion of the cervical spine is a distinctive characteristic of the cervical vertebrae. Cervical spinal nerves have a few unique protective mechanisms. First, the free mobility of the nerve sleeve, ganglion and spinal nerve within the foramen, allows the neural structures adapt to movements of the cervical spine without deformation or injury71). A second feature is the adherence of the spinal nerves and the transverse process at the level of lower cervical spine. When traction force affects the spinal nerve, this adherence of the spinal nerve and the transverse process is torn primarily. If greater traction force affects, the root sleeve is pulled into the intervertebral foramen and tearing occurs before the root. For these reasons, considerable force on the shoulder and upper arm is required to carry sufficient power to cause root avulsion.
Closed trauma is the most common cause of adult traumatic BPI. Most common mechanism of closed trauma causing BPI is compression or traction. BPIs caused by compression may be accompanied by fractures or dislocations of the clavicle or the head and neck of humerus. Gradual compression results from the postoperative edema or fibrosis is also one of the hypotheses to explain BPI occurrence, although there is controversy43).
In BPIs caused by traction, the nerve may be injured, avulsed from the root, or significantly stretched70). Traction-related injuries can be resulted from violent widening of the scapulo-humeral angle accompanied by the shoulder dislocations and fractures of the humerus, which cause pressure on the infraclavicular neurovascular bundle above the humeral head, and injury of the infraclavicular plexus. One of the examples is when someone falls on a laterally hyperabducted and internally rotated arm and the movement of the scapula is blocked by the ground, and infraclavicular plexus is stretched over the humeral head53). Because axillary artery located too close to the medial, lateral and posterior cord, accompanying rupture of axillary artery has been reported by up to 50% of the infraclavicular plexus injuries21). Supraclavicular brachial plexus lesions are more frequent rather than infraclavicular lesion. The most commonly injured sites are the roots and trunks in comparison to the rest parts of the brachial plexus. Root avulsions exist in 75% of cases of these supraclavicular injuries54).
The patient’s position and the location of the upper limb when the injury occurs is the most important point to understand the mechanism of BPI7). Different position and location of the upper limb will lead to different injury mechanism, because tension could be applied to various roots. If the upper limb is adducted, the greatest tension and mechanical stress will affect the upper roots. One of the instances is the motor cycle accident. After someone is thrown from their motorcycle and dropped to the ground by the shoulder, the head is aggressively flexed away from ipsilateral, downwardly depressed shoulder. This results in violent widening of the shoulder-neck angle, and the upper brachial plexus is stretched between 2 fixed points and avulsed. It results in rupture or stretch of the upper roots (C5–C7), but the lower roots (C8, T1) are preserved. When the upper limb is elevated and the traction force affects the arm or the trunk, substantial tension force will affects the lower roots. One of the instances is when someone hangs on to a tree branch with one arm. In this situation, the upper limb is abducted and forced behind the back, and great tension force will affect all of the roots. Over time, cellular proliferation occurs and closes the tear, and the meningocele, a pouch like extension, appears.
3. Classification
BPIs can be divided into three types; preganglionic lesion, postganglionic lesion, and a combination of both. Whether the continuation of the root and the spinal cord is preserved is a critical factor in determining the treatment strategy. Preganglionic injuries involve the nerve roots avulsion, and imply that the rootlets that connect the peripheral nerve to the central nervous system have been disrupted. Therefore, the root that is affected cannot be used as a nerve source for reconstruction, and alternative methods of reconstruction are necessary. Whereas, postganglionic injuries involve nerve ruptures or discontinuation distal to the sensory ganglion, and imply that the connection to the central nervous system is intact and the nerve can be used as a source of axons81).
4. Clinical Manifestation
The level of lesion can be analogized by clinical manifestations, such as active and passive movements of the shoulder, upper arm, lower arm and hand and wrist, through a full range of movements. Muscle grading system such as LSUHSC(Louisiana State University Health Science Center) grades and MRC (Medical Research Council) grades has been used to evaluate the power of muscles. An upper brachial plexus lesion (C5, C6) leads to paralysis of the shoulder muscles and biceps. Paralysis of the shoulder muscles accompanied by an inability of arm abduction, or weakness of the rhomboid muscle indicates a lesion at the level of C5. If elbow flexion and wrist extension is marked impaired or winging of the scapula is detected, C6 involvement should be considered. When C7 is involved, some of the wrist and forearm muscles are affected. A lower brachial plexus lesion (C8, T1) causes paralysis of the forearm flexor and the intrinsic muscles of the hand52). Avulsion or damage of the C8 and T1 nerve roots from which the cervical sympathetic chain arises cause Horner syndrome, which is characterized by ptosis, meiosis, anhidrosis of the cheek and enophthalmos. Because T1 sympathetic ganglion is proximal to T1 nerve root, investigators should inspect all patients with BPI for signs of Horner’s syndrome. As well as motor function, sensory dermatomal distribution and reflexes should be checked. Purcussing a nerve, so called Tinel’s sign, is particularly helpful in identifying the site of injury. If percussion the nerve arouses acute pain, this suggests a rupture. The proceeding of Tinel’s sign is a sign suggesting the recovery of lesion54). Various types of neurologic and functional loss of BPI were summarized at Table 1.
5. Diagnosis
1) Radiographic Evaluation
To rule out coexistent fractures of the spine, ribs, clavicle, scapula, or bones within the affected extremity, radiographic examination of the cervical spine, involved shoulder and extremity, and chest should be performed. Investigators can ascertain the presence of the first and second rib fractures which indicate potential damage to the overlying brachial plexus using standard chest AP X-rays. Transverse process fractures of the cervical vertebrae can be identified by cervical radiograph, and indicate possible root avulsion at the level. Inspiratory-expiratory chest films, ultrasound of the diaphragm or fluoroscopy provides information about the phrenic nerve function and potential injury to the C5 nerve root, as the phrenic nerve receives contributions from C3 to C5.
Patients with BPI represent 10% to 25% incidence of accompanying arterial injury31). If physical examination demonstrates abnormal radial or ulnar pulses, vascular imaging such as arteriography or magnetic resonance angiography is indicated.
(1) Myelography
Myelography is a simple and economical diagnostic method. It is available in most hospitals, but involves disadvantages such as radiation exposure and adverse effects from contrast material. It enabled demonstration of the nerve root avulsions with a water soluble contrast agents. Myelography was the traditional mainstay for diagnosis of brachial plexus lesions20). The diagnostic accuracy is known to be only 37.5%, although accuracy at the level of C8 and T1 was 75%46). The diagnostic accuracy of myelography was lower at the level of C5 and C6, probably due to the narrow subarachnoid space at these levels. However, the sensitivity of myelography has been superior to which of computed tomography (CT) myelography for evaluation of the lesions at the level of C8 and T1, because shoulder artifacts could obscure a CT view at these level46,79).
(2) CT Myelography
Nowadays, CT myelography is the current gold standard diagnostic method for avulsion injuries33,34). Using CT myelography, ventral and dorsal nerve roots can be evaluated separately and intradural nerve defects is detected. The great advantage of CT myelography compared to myelogram is the ability to detect the partial avulsions at C5 and C6 levels, with an overall accuracy of 75%46). Carvalho et al.14) performed direct surgical examination of the intradural nerve roots through multiple hemilaminectomy and achieved an accuracy of 85% using 3 mm sections11,32,46) CT myelography at 3 to 4 weeks after injury is recommended, because the clots in the area of injury that would otherwise displace the dye might disappear at that time56). The presence of a pseudomeningocele at 3 to 4 weeks after injury highly suggests root avulsion. Traumatic meningocele is a meaningful suggestive sign of a preganglionic lesion, although it is not a specific finding. Nerve root avulsion can occur without a meningocele, and a meningocele can exist without nerve root avulsion60). Absence of roots is another important sign suggesting preganglionic lesion. Fig. 2B and C shows CT myelography representing a traumatic meningocele with nerve root avulsion.
(3) MRI
MRI has shown less accurate imaging compared with CT myelography. In the study of Carvalho et al.14) the accuracy of MRI was only 52% and it did not provide adequate information for diagnosis in over 30% of cases. The relative advantage of MRI over CT myelography is the non-invasiveness and much higher image quality of the brachial plexus. MRI is also useful for visualization of the postganglionic brachial plexus, and for distinguishing from benign and malignant tumorous lesions81). Signal intensity changes of the spinal cord are accompanied in 20% of patients with preganglionic injuries. It provides excellent evaluation of edema in the acute phase, myelomalacia in the chronic phase, fibrosis, or neuroma formation in the post-ganglionic plexus61). Contrast-enhanced MRI is helpful to identify functionally impaired nerve roots with preserved native anatomy and avoid abortive reconstructive procedures. Abnormal enhancement of paraspinal muscles which started as early as 24 hr after injury is caused by expansion of the vascular bed and the extracellular space. It is an accurate indirect sign of root avulsion injury. Another advantage of MRI is detection of meningocele. Myelography may not demonstrate meningocele if connection between the CSF space and the meningocele is blocked by cellular proliferation. In contrast, MRI does not rely on the presence of a contrast agent within the CSF space. It can reveal fluid collection that doesn’t have connection with the CSF. Fig. 2A shows BPI with traumatic meningocele which is represented as high signal in T2-weighted MRI.
(4) Magnetic Resonance Neurography(MRN)
The development of MRI sequences shows even the detailed part of the plexus. The MRN is composed of T1- and T2-weighted imaging (WI), short-tau inversion recovery (STIR), 3-dimensional (3D) STIR SPACE and 3D T2 SPACE sequences. It is non-invasive and allows to identify both proximal and distal parts of the brachial plexus. Modern 3D MRN sequences are useful for identifying the extent of injury and finding the optimal treatment strategy15,75). T1-WI help to identify the anatomical structure and morphology of the plexus. Axial T2-WI using fat-suppression are useful for identifying findings related to the level of injury. Sagittal STIR images can be used to identify plexus components and their relationship to surrounding structures such as subclavian vessels. In the coronal 3D STIR SPACE sequence, the plexus appears to be bright as the background fat is homogenously suppressed. Isotropic multi-planar and curved planar reconstruction enhanced by maximum intensity projection (MIP) shows the abnormality of the injured plexus. MRN helps to classify BPI into pre-ganglionic, post-ganglionic, or mixed. Approximately 20% of pre-ganglionic injuries show altered signal intensity of the ipsilateral spinal cord due to edema, hemorrhage, and myelomalacia75). T2 hyperintense signals are associated with edema and myelomalacia, while T2 hypointense signals are evidenced by blood degradation products when hemorrhage is present. Post-ganglionic plexus injuries on MRI appear with signs that signify neuropraxia, axonotmesis or neurotmesis. When there is a stretch injury, thickened plexus components can be seen in the T2-WI. Recent modalities such as diffusion tensor imaging (DTI) continue to evolve28). Nerve tractography images may help to obtain additional information in the diagnosis and treatment of BPI.
(5) Ultrasonography(USG)
USG of the brachial plexus has been used as guidance for brachial plexus anesthesia. Recently, it was proposed as a technique to evaluate the post-ganglionic brachial plexus47,66). The potential advantages of ultrasound include high soft tissue resolution and the ability to identify each part of the plexus as it passes in an oblique plane through the base of the neck. However, the reliability of this technique in case of postganglionic injuries should be elucidated.
In recent years, there have been attempts to utilize new imaging techniques for diagnosis and determine the effectiveness after treatment of BPI. Animal study showed ventral horn shrinkage at the level of spinal MRI by neuronal and glial changes after avulsion35). Functional MRI has also been used and demonstrated brain plasticity and compensatory mechanism by dynamic changes in resting state networks of the brain after BPI and repair11). Recent study revealed that assessment of muscle atrophy and fatty degeneration using quantitative three-point Dixon MRI sequences reflects active flexion and muscle force after BPI24).
2) Electrophysiology Studies(EPS)
Electrodiagnostic studies reveal subclinical injuries and recognize subclinical recovery. Electromyography (EMG) is an electrodiagnostic tool to evaluate the level of electrical activity generated by skeletal muscle. EMG is helpful to confirm a diagnosis, localize the level of the lesion, estimate the severity of axon loss, and completeness of the lesion. It also helps to distinguish preganglionic from postganglionic lesions. Sensory nerve action potentials (SNAPs) are specifically important in localizing the lesion as either pre- or postganglionic. The cell body of the sensory neuron locates within the dorsal root ganglion; therefore, SNAPs are preserved in lesions proximal to the dorsal root ganglions due to ongoing postganglionic electrical activity. The patient with a preganglionic lesion will have evidence of SNAPs despite the extremity being insensate in that nerve distribution. The SNAPs are not present in postganglionic or combined pre-and postganglionic lesions.
In closed traction injuries, to perform EMG within 4 to 6 weeks after the injury is usually recommended to look for spontaneous recovery. Serial EPS with repeated physical examinations is necessary to identify the progression of recovery, and to predict the potential of surgical exploration of the BPI lesion33,67). The presence of active motor units, the appearance of early potentials, and a decrease in the number of fibrillation potentials indicate recovery and a good prognosis.
6. Management
1) Initial Management
A detailed history of the injury and associated injuries should be elucidated in the first visit. A detailed physical examination assessing both the motor and the sensory components of every muscle group innervated by the brachial plexus is also mandatory; muscle power is estimated by British Medical Research Council muscle grading system and sensory by measuring dermatomal sensation and 2-point sensation in the digits. Tinel’s sign in the supraclavicular and infraclavicular plexus should be confirmed, which can be an indicator implicating whether the BPI is distal to the spinal foramen or not (post-ganglionic). Investigators should examine passive and active ranges of motion of the shoulder, elbow, forearm, and wrist, as well as reflexes. Specific physical signs suggesting differentiation of the limb, including Horner’s sign or severe pain in an anesthetic extremity, indicate that the BPI is proximal to the spinal foramen (preganglionic). Palpation of radial and ulnar pulses is required to screen for concomitant vascular injuries. Due to 2% to 5% incidence of spinal cord injury with BPIs, the examination for potential spinal cord injury should be evaluated59).
Besides clinical finding, electrophysiological and radiologic finding are also considered when considering operation40,48). The EPS, such as peripheral and paraspinal musculature EMG as well as sensory nerve conduction studies (NCS), provides important information. One of the imaging studies currently used is myelography. If brachial plexus palsy persists, myelography should be performed within 1 to 2 months after injury. The existence of one or more large pseudomeningoceles usually suggests root avulsion56).
The injury mechanism, the time from injury, the injury type (pre vs postganglionic), the priorities of treatment, and the concomitant injuries all should be considered in the decision-making process.
2) Conservative Management
If diagnostic EMG suggests that the damage is non-degenerative, conservative management is indicated. Conservative managements include the use of assistant device such as slings and splints to prevent uncontrolled positional movement of the paralyzed limb which can hinder the quality of life. Extensive physical therapy is also recommended as part of conservative management. Passive range of movements (PROMS) can be used on a daily basis to maintain joint mobility and muscle strength of arm. Electrical stimulation and therapeutic massage for edema and scar management are other conservative options39). Adequate pain relief should be considered for each patient to minimize patients’ discomfort and maximize physiotherapeutic potential.
3) Surgical Treatment
If there is no evidence of spontaneous recovery within 6 months of injury, a reconstructive plan should be formulated. Although debatable, most brachial plexus surgeons would agree that recovery of elbow flexion is the most important function, followed by shoulder abduction. Although recovery of motor function is a priority in brachial plexus reconstruction, restoration of protective sensation is also important for prehensile function, prevention of injuries, and even modulation of the pathogenesis of the deafferentation pathway of pain. Each of these elements can improve the patient’s quality of life.
(1) Indications and Timing for Surgery
The optimal time between injury and surgery is one of the most important factors responsible for the surgical results. Early operation might not allow sufficient time for spontaneous reinnervation; however, too late operation after 6 to 18 months of denervation can lead to failure of the motor end plate and thus failure of reinnervation78). In general, the optimal time of surgical intervention is regarded as 3 to 6 months after injury37).
The mechanism of injury determines the appropriate timing of surgical intervention. Most injuries result from vascular causes require emergency surgery. If there is complete C5 and T1 avulsion injuries, early exploration within 1 to 2 weeks is recommended44). When root avulsion is highly suspicious, early exploration and reconstruction between 3 and 6 weeks is indicated67). If there has been no functional recovery or no change in the physical examination or EMG, delayed exploration at 12 weeks after injury is recommended.
In sharp open injuries, immediate exploration and primary repair is required. In blunt open injuries, delayed exploration with tagging of the lacerated nerves might be required. By 3 to 4 weeks after injury, the nerve injury will have demarcated, and nerve repair outside the zone of injury is possible. Low-velocity gunshot wounds should be managed conservatively. On the other hand, high-velocity gunshot wounds require surgical exploration. The best operative timing for closed traction injuries is 4 to 5 months after injury, though the exact timing of surgery remains controversial.
(2) Surgical Options
Operative options used in BPI include nerve grafting, neurotization (nerve transfer), and other brachial plexus reconstructive techniques including the transplantation of various structures41).
(3) Nerve Grafting
Nerve grafting is a procedure which is used to make connectivity of the ruptured nerves in postganglionic injury. Nerve repair with grafting allowed the regeneration of axons down original pathways to reinnervate multiple muscles. It is theoretically the best surgical strategy; however, whether geography and structure of the regenerating fibers simulates the native sensory and motor fiber distinction remains unclear. Nerve grafting cannot be used in pre-ganglionic injuries, because a length of proximal nerve is required. In postganglionic injuries, spontaneous recovery with conservative management is usually expected if lesions in continuity are nondegenerative or fascicles are intact. However, postganglionic lesions with the nerve fiber destruction could be recovered by nerve grafting. The most commonly used donor nerve is both sural nerves; it can be as long as 30 cm5). Common examples of interpositional nerve grafting include coaptation of C5 root to suprascapular nerve or axillary nerve (for shoulder abduction), C6 to musculocutaneous nerve (for elbow flexion), and C7 to triceps or radial nerve (for elbow extension and wrist extension) (Fig. 3).
(A) C5 preganglionic & C6-T1 postganglionic injury. C5 preganglionic & C6-T1 postganglionic injury and (B) repair with cranial nerve XI to superior cluneal nerves; descending cervical plexus to the posterior division of the upper trunk (UT); C6 graft repair to the anterior and posterior divisions of the UT; C7 graft repair to the anterior and posterior divisions of the middle trunk; and C8 and T1 graft repair to anterior and posterior divisions of the lower trunk (drawn by Kim IS).
There was no relationship between the length of the nerve grafts and the surgical outcome after the brachial plexus reconstruction surgery in the study reported in 1970s63). One of the hypotheses is that the graft vascularization occurs from even the surrounding tissue, as well as the proximal nerve donor or distal nerve stump. However, Chuang et al.17) compared grafts shorter than 10 cm with those longer than 10 cm, and concluded that graft length was an important factor in functional outcome after nerve transfer for elbow flexion recovery. Patients treated with shorter grafts represented a considerably higher reinnervation rate than those with longer grafts. This finding could be explained by that the patients who required longer nerve grafts might have more extensive brachial plexus lesion and more severe proximal and/or peripheral nerve fibrosis.
Surgical technique has been demonstrated as an important factor affecting the surgical outcome6,25,64). A weak coaptation and tension at the nerve union site cause the increase of scar tissue, fibrosis and granulomatosis, which may worsen the redevelopment of growing axons64).
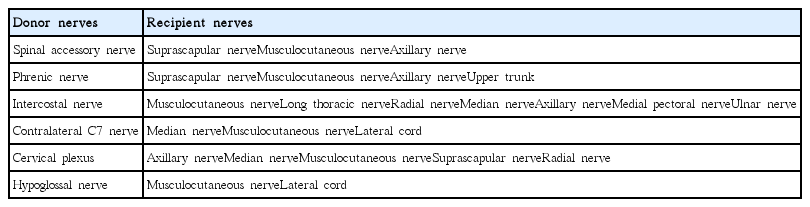
4) Neurotization(Nerve transfer)
If the injury is preganglionic, reconstruction using nerve transfers could be helpful. The objective of the nerve transfer is not reinnervation of the brachial plexus in its original anatomy. Instead of that, lesser important nerve(donor nerve) is attached to the ruptured distal stumps; it is sacrificed to obtain a more advantageous nerve function (recipient nerve)62). Table 2 represents possible donor and recipient nerves. It represents promising surgical outcome with restoring useful limb function in the following situations; preganglionic injuries in which nerve root stumps are not available, or long-lasting injuries requiring long grafts for repair10,50,51). Theoretically, nerve transfer is useful to restore axonal input into the single denervated target. One of the advantages is the anatomic proximity of the donor and recipient nerve, and reduced operative time and the unnecessity of an intervening graft are also benefits of the nerve transfer12,70).
In general, biceps muscle function and shoulder function are regarded as to have the priority of nerve repair8,45,52). Intercostal-musculocutaneous nerve transfer is usually used to regain elbow flexion, and spinal accessory nerve-suprascapular nerve transfer is used to obtain functional recovery of the shoulder8). Various nerves which have been used as donor include the phrenic nerve, regional nerves such as C3 and C4, and other constituents of the brachial plexus for plexoplexal transfers and contralateral C7 transfers (Fig. 4, 5)30,70). Nerve transfers can also be used to innervate and power free-functioning muscle transfers.
(A) C5, C6 preganglionic & C7 postganglionic injury. C5, C6 preganglionic & C7 postganglionic injury and (B) repair with nerve transfers of cranial nerve XI to superior cluneal nerves; descending cervical plexus to the posterior division of the upper trunk; and medial pectoral nerve to musculocutaneous nerve (drawn by Kim IS).

(A) C5, C6 preganglionic & C7, C8 postganglionic injury. Depicted are C5, C6 preganglionic & C7, C8 postganglionic injuries, and (B) repair with nerve transfers of cranial nerve XI to superior cluneal nerves; descending cervical plexus to the posterior division of the upper trunk; and intercostal nerve to the musculocutaneous nerve (drawn by Kim IS).
(5) Future Prospects
Nerve root repair and re-implantation ventral roots into spinal cord are emerging techniques for BPI, presenting promising results13). After the exposure of the spinal cord by multiple laminectomy, a graft is inserted into a slit in the spinal cord and connected to the avulsed roots. However, further clinical study is required before using this technique as standard procedure.
(6) Surgical Outcome
Surgical results of BPI have been reported by many investigators4,9,23,34,49,72). Most patients with BPI have obtained a recovery of useful arm motor function after surgical reconstruction8). Operative repair technique was an important factor in brachial plexus reconstruction and recovering the use of an arm. In the study of Nagano et al.56), elbow flexion was recovered in more than 80% of patients under 40 year-old who underwent intercostal nerve transfer within 6 months of injury. Almost 60% of the patients obtained satisfactory outcome after brachial plexus reconstruction with nerve grafting. The outcome of neurotization or nerve transfer was also satisfactory in 40% of the patients23). Most patients were satisfied with their improved quality of life after surgical reconstruction. Only one-fifth of patients experienced permanent total disability after surgical reconstruction for BPI16).
4) Pain after BPI
Pain, one of the most negatively affecting factors on the quality of life patients with BPI, is a common symptom after BPI, accounting for 67% to 71%14,74). Pain after BPI is usually neuropathic, with rates of neuropathic pain reported as high as 95%18,19,77). It is usually caused by trauma or traumatic neuropathy to the musculoskeletal system, but other kinds of pain associated with nociceptive pain and complex reginal pain syndrome can also occur. Nociceptive pain results from tissue injury that activates the pain receptor, and also associated with inflammation, which often leads to peripheral hyperexcitability of the nociceptive system. Causes of nociceptive pain associated with BPI include myofascial pain, tendinitis, postoperative lesion, and muscle overload due to unbalanced movement and joint pain. Also, there have been reports that central injury-related mechanism contributes to pain after BPI. Central sensitization, a mechanism contributes to the amplification and chronification of pain, increases the gain of injured somatosensory systems and the perception of pain stimuli, lowers the threshold, and increases the central processing of the peripheral input, causing secondary hyperalgesia beyond the denervated area58,80).
Pain after BPI is often irresponsible to pharmacological therapy. Approximately 25% of patients experience severe neuropathic pain that lasts for years57). Neuropathic pain is more severe and lasts longer than other types of chronic pain, and often required surgical treatment with the neuromodulation or neuroablative techniques73). One of the neurosurgical treatments for post-BPI pain is dorsal root entry zone lesioning, which has shown a significant effect on paroxysmal pain. Two-thirds of the patients have a long-term effect, but about 10% experienced dysesthesia and ipsilateral leg weakness1,26). Motor cortex stimulation (MCS) is not effective for paroxysmal pain, but is known to be very effective for continuous pain3,42). Spinal cord stimulation (SCS) is also reported to be effective in some patients27). In a comparative study of a small number of phantom limb patients, deep brain stimulation was reported to be more effective than MCS or SCS36). However, further randomized, controlled, and clinical trials are need for neuromodulation treatment.
CONCLUSION
Traumatic BPIs in adult arise from various traumatic or non-traumatic mechanisms, and their frequency has been increasing. BPIs commonly affect the quality of life and cause catastrophic injury. Early recognition of the mechanism and level of the injury is principal in establishing early treatment leads to better outcome. A thorough clinical examination is essential to obtain accurate diagnosis. Recent progress in radiologic and neurosurgical techniques has steadily improved the outcome of the patients with BPI. CT myelography still remains the gold standard diagnostic method for BPI. However, MRI also has important role in identifying the physical continuity of nerve roots and spinal nerves. Only about 40 to 50 years ago, treatment of BPIs was considered a wasted endeavor by many leaders in the peripheral nerve field. However, advances in surgical techniques and further understanding of nerve physiology have led to improved outcomes. The current trend of treatment strategy for BPI is surgical reconstruction by nerve graft of nerve transfer procedures.